Giant Cell tumor of the Zygomatic Arch in a Pediatric Patient: Rare Case Report
Tumor de Células Gigantes do Arco Zigomático em um Paciente Pediátrico: Relato de Caso Raro
Tumor de Células Gigantes del Arco Cigomático en un Paciente Pediátrico: Informe de un Caso Raro
doi: https://doi.org/10.32635/2176-9745.RBC.2022v68n2.1880
Jhulia Farinha Maffini1; Maria Eduarda Turczyn De Lucca2; Leonardo Cesar Ferreira Antunes3; Felipe Antonio Torres Mazzo4; Carlos Eliseu Barcelos5; Rodrigo Leite de Moraes6; Eduardo Talib Bacchi Jaouhari7; Milena Massumi Kozonoe8; Rosângela Stadnick Lauth de Almeida Torres9
1-3,9Universidade Positivo (UP). Curitiba (PR), Brazil. E-mails: jhuliamaffini@gmail.com; mariatdelucca@gmail.com; leonardocfa@hotmail.com; rslatorres@gmail.com. Orcid iD: https://orcid.org/0000-0003-0930-7087; Orcid iD: https://orcid.org/0000-0002-7625-8193; Orcid iD: https://orcid.org/0000-0002-3963-3716; https://orcid.org/0000-0002-8974-3323
4Pontifícia Universidade Católica do Paraná (PUCPR), Escola de Medicina. Curitiba (PR), Brazil. E-mail: felipetorresmazzo@hotmail.com. Orcid iD: https://orcid.org/0000-0001-5378-1558
5-8Hospital Erasto Gaertner (HEG), Departamento de Neurocirurgia. Curitiba (PR), Brazil. E-mails: cbarcelos@hotmail.com; rodrigo.neuro@hotmail.com; eduardotalib@gmail.com; mikozonoe@gmail.com. Orcid iD: https://orcid.org/0000-0001-8858-3017; Orcid iD: https://orcid.org/0000-0001-5231-0447; Orcid iD: https://orcid.org/0000-0002-8964-6566; Orcid iD: https://orcid.org/0000-0002-5239-8175
Corresponding author: Jhulia Farinha Maffini. Avenida Presidente Getúlio Vargas, 2840 – Água Verde. Curitiba (PR), Brazil. Cep 80240-040. E-mail: jhuliamaffini@gmail.com
ABSTRACT
Introduction: A giant cell tumor (GCT) is a rare tumor, usually benign, which can be locally aggressive, with an almost unknown incidence in the skull. Case report: Case report of a pediatric patient diagnosed with Ewing’s sarcoma (ES) and later GCT when sought medical care for an increased volume in the zygomatic arch and the right preauricular region. Imaging exams showed an expansive lesion in the zygomatic and squamous portion of the right temporal bone, with an extradural intracranial component in the middle fossa, with no evidence of infiltration. From the anatomopathological view, fusocelullar neoplasia was seen. The CD68 marker was positive and the S100 marker was negative. Tumor resection by microsurgery was performed. The patient remains in follow-up, with imaging exams at neurosurgery and orthopedics, the latest magnetic resonances of the skull showing a reduction in the size of the lesion. In addition, the patient did not submit to adjuvant therapy and is currently without complaints. Conclusion: This is an important case due to its rarity and clinical data that contributes for the understanding of the pathologies presented, allowing that, in the future, new studies are able to optimize the treatment, and the prognosis for these patients.
Key words: giant cell tumor of bone; cranial fossa, middle; skull neoplasms; case reports.
RESUMO
Introdução: O tumor de células gigantes (TCG) é raro, geralmente benigno, e pode ser localmente agressivo, com incidência quase desconhecida no crânio. Relato do caso: Paciente pediátrico com diagnóstico de sarcoma de Ewing (SE) e posteriormente de TCG, quando procurou atendimento médico por conta do aumento de volume em arco zigomático e região pré-auricular à direita. Os exames de imagem evidenciaram lesão expansiva em porção zigomática e escamosa do osso temporal à direita, com componente intracraniano extradural em fossa média, sem evidências de infiltração. Do ponto de vista anatomopatológico, observou-se neoplasia fusocelular. O marcador CD68 foi positivo e o marcador S100, negativo. Realizou-se microcirurgia para ressecção do tumor. O paciente permanece em acompanhamento com exames de imagem nos serviços de neurocirurgia e ortopedia, com as últimas ressonâncias magnéticas de crânio mostrando redução no tamanho da lesão. Além disso, não realiza terapia adjuvante e atualmente não apresenta queixas. Conclusão: Este é um caso importante em razão da sua raridade e dos dados clínicos que agregam informações sobre as patologias apresentadas, permitindo que, no futuro, novas pesquisas possam otimizar o tratamento da referida neoplasia e o prognóstico desses pacientes.
Palavras-chave: tumor de células gigantes do osso; fossa craniana média; neoplasias cranianas; relatos de casos.
RESUMEN
Introducción: El tumor de células gigantes (TCG) es un tumor raro, generalmente benigno, que puede ser localmente agresivo, con una incidencia casi desconocida en el cráneo. Relato del caso: Paciente pediátrico diagnosticado con sarcoma de Ewing (SE) y posteriormente con TCG, cuando procuró atención médica por aumento de volumen en arco cigomático y región preauricular derecha. Los exámenes de imagen mostraron una lesión expansiva en la porción cigomática y escamosa del temporal derecho, con componente intracraneal extradural en la fosa media, sin evidencias de infiltración. Desde el punto de vista anatomopatológico, se observó neoplasia fusocelular. El marcador CD68 fue positivo y el marcador S100 negativo. Se realizó microcirugía para resecar el tumor. El paciente permanece en seguimiento con exámenes de imagen en los servicios de neurocirugía y ortopedia, con las últimas resonancias magnéticas de cráneo mostrando una reducción en el tamaño de la lesión. Además, no se somete a terapia adyuvante y actualmente no tiene quejas. Conclusión: Este es un caso importante por su rareza y datos clínicos que agregan informaciones sobre las patologías presentadas, permitiendo, en el futuro, nuevas investigaciones para optimizar el tratamiento de la neoplasia referida, y el pronóstico de estos pacientes.
Palabras clave: tumor óseo de células gigantes; fosa craneal media; neoplasias craneales; informes de casos.
INTRODUCTION
A giant cell tumor (GCT) is usually a benign tumor, which can be locally aggressive. They account for 5% of bone tumors, only 2 to 5% of these cases occur in the pediatric group whose age-range is 13-19 years. The treatment of choice is surgical1-3. Monitoring the patient after the end of treatment is essential, as GCTs have high recurrence rates4.
Case report about a GCT in a child localized in the zygomatic arch and in the squamous portion of the right temporal bone.
The Institutional Review Board of “Centro de Projetos de Ensino e Pesquisa (CEPEP)” of “Hospital Erasto Gaertner”, Curitiba, Brazil approved the study, CAAE number 87548518.2.0000.0098. The study patient signed the Informed Consent Form (ICF).
CASE REPORT
Male patient, 12 years old, previously diagnosed and treated for Ewing’s sarcoma in the left hip, returns to the pediatric oncology service of Hospital Erasto Gaertner, Curitiba, PR, complaining of swelling in the zygomatic and right preauricular region, detected by the family after one month of a local trauma. The lesion was difficult to delimit upon unpainful palpation.
A skull computed tomography (CT) showed a solid destructive lesion, compromising the right zygomatic arch, extending to the ipsilateral temporal bone, where it was determined intracranial compartment invasion. Anatomopathological analysis of a biopsy specimen showed gigantocellular proliferation associated with reactive osteoid neoformation.
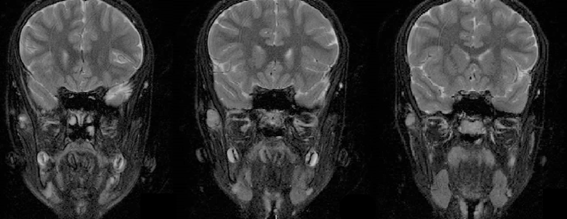
Magnetic resonance imaging (MRI) was performed for surgical planning (Figure 1), showing an expansive bone lesion affecting the zygomatic arch and squamous portion of the right temporal bone, measuring about 4 cm in its longest axis, with a small extradural intracranial component in the middle cranial fossa, with no evidence of infiltration or dural thickening. Therefore, the patient underwent microsurgery for total tumor resection.
|
|
|
Figure 1. MRI of the skull showing an expansive bone lesion, measuring approximately 40 mm on the longest axis of the axial plane, compromising the zygomatic arch and squamous portion of the right temporal bone, with a small extradural intracranial component in the middle cranial fossa, compatible with neoplasia with aggressive characteristics |
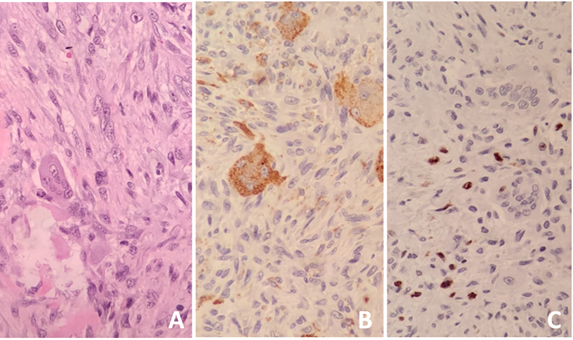
The anatomopathological diagnosis of the excised lesion showed fusocelullar neoplasia with giant cells with foci of bone neoformation. Immunohistochemistry showed positivity for CD68 (Figure 2) and negativity for S100, closing the diagnosis of GCT. One month after surgery, the control skull CT scan showed two lesions, one on the inner face of the middle third of the zygomatic arch, measuring 9x8x6 mm, and another lesion in the transition between the posterior portion of the zygomatic arch and squamous portion of the right temporal bone, measuring 13x7x5 mm, with suspicion of recurrent or residual injury.
|
|
|
Figure 2. Anatomopathological diagnosis. A. Excised lesion showing fusocelullar neoplasia with giant cells with foci of bone neoformation, compatible with giant cell tumor (H&E); B, C. Immunohistochemistry showed positivity for CD68 and Ki67 (proliferation index), respectively |
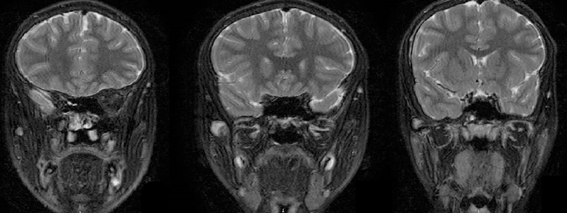
The patient returned to a new MRI in 3 months, which showed the same irregular expansive lesion in the proximal portion of the right zygomatic arch, measuring about 30x13x14 mm, which may represent an area of confluence of the lesions identified in the previous examination. Another skull MRI (Figure 3) 9 months after surgery showed a slight reduction of the lesion, now measuring 19x5x19 mm. A possible relapse of the injury was again suggested.
|
|
|
Figure 3. Lesion with expansive effect and lobulated contours, located in the proximal aspect of the right zygomatic arch, measuring about 19x5x19 mm |
The patient continues to be monitored. Until the beginning of the year 2020, he had no complaints, without recurrence signs of the ES and monitoring of the dimensions of the GCT of the zygomatic arch.
DISCUSSION
GCTs are considered primary bone neoplasms, and, for pediatric cases, the most common implantation sites are the longest bones. There is suggestion that involvement of the temporal bone occurs in approximately 1 in 546 cases of GCT, the extension to the infratemporal fossa is extremely uncommon3. It is important to note that GCT has its peak of incidence between 30-40 years old, more common in females. Even though the incidence of cranial GCT is rare in children, it’s still more typical than in a male adult in this site (the ratio is 2:1 female in the first and second decade of life for 1 male adult). The clinical condition is variable. In cases of involvement of the axial skeleton, there may be complaints of pain, edema, deformities, and restricted mobility. When present in the temporal bone, a patient may complain of retroauricular pain, hearing loss, and weakness of facial muscles1,3,4.
Some differential diagnoses should be considered, such as giant-cell reparative granuloma, aneurysmal bone cyst, chondrodysplasia, metastatic lesions, and Ewing’s sarcoma4.
The imaging exams were important to determine the extent of the lesion and support the diagnosis. Histologically, it is a heterogeneous tumor, presenting giant multinucleated cells resembling osteoclasts and spindle cells. In immunohistochemical analysis, CD68 and CD163 markers may be present1,4.
The first line of treatment for cranial GCT is surgical resection, with subsequent reconstruction. Adjuvant treatment can be associated to reduce the risk of neoplasm recurrence4-6. The patient must be monitored after the end of treatment, as GCTs have recurrence rates of 40-60%4.
According to the few information available in articles, the first and only treatment line implemented in the case was surgical. After being discharged, he continued in follow up with regular skull MRI and other imaging tests, the most recent MRIs showing a reduction of the lesion’s dimensions, which had previously increased. A possible recurrence continues to be questioned.
A few similar cases were found while investigating the case. One of them, according to Elder et al.4, was a 2-year-old girl diagnosed with GCT of the right temporal bone, affecting the dura mater as well. The treatment of choice was microsurgery, similar to the current case. After 13 months of follow-up, there were no signs of recurrence. In the same article, the authors reported the case of a 7-week-old female infant diagnosed also with a GCT at the left temporal bone, involving the left external and internal auditory canal, the confluence of sinuses, parotid gland and cerebellopontine angle without metastasis. The treatment was a gross-total resection of the mass. In a 11-month post-operative follow-up, there were no signs of recurrence, but a persistent left facial palsy was detected4.
CONCLUSION
This is an important case due to its rarity, new clinical data about the pathologies and the patient’s survival. Possibly, future studies may discuss the optimization of the treatment of these neoplasms, mainly of GCTs of the zygomatic arch, and consequently, the prognosis of these patients.
CONTRIBUTIONS
Jhulia Farinha Maffini and Leonardo Cesar Ferreira Antunes contributed for the article drafting and data acquisition; Maria Eduarda Turczyn De Lucca contributed for the article drafting, review and editing;, Felipe Antonio Torres Mazzo contributed for the article drafting, review, editing and figures; Carlos Eliseu Barcelos contributed for the study conception and investigation; Rodrigo Leite de Moraes and Eduardo Talib Bacchi Jaouhari contributed with data collection and investigation; Milena Massumi Kozonoe contributed with data collection; Rosângela Stadnick Lauth de Almeida Torres contributed for the supervision. All the authors reviewed, read and approved the final version to be published.
CONFLICTS OF INTEREST
There is no conflict of interest to declare.
FUNDING
REFERENCES
1. Federman N, Brien EW, Narasimhan V, et al. Giant cell tumor of bone in childhood: clinical aspects and novel therapeutic targets. Pediatr Drugs. 2014;16(1):21-8. doi: https://doi.org/10.1007/s40272-013-0051-3
2. Roberts DS, Faquin WC, Deschler DG. Giant cell tumors of the temporal bone and infratemporal fossa: a case report and review of the literature. Laryngoscope. 2010;120(Suppl 4):S180. doi: https://doi.org/10.1002/lary.21644
3. Roberts DS, Faquin WC, Deschler DG. Temporal bone giant cell tumour: report of a second primary giant cell tumour of the temporal bone and infratemporal fossa. B-ENT [Internet]. 2011 [cited 2021 Apr 20];7(4):301-3. Available from: http://www.b-ent.be/en/temporal-bone-giant-cell-tumour-report-of-a-second-primary-giant-cell-tumour-of-the-temporal-bone-and-infratemporal-fossa-16500
4. Elder JB, Berry C, Gonzalez-Gomez I, et al. Giant cell tumor of the skull in pediatric patients: report of two cases. J Neurosurg. 2007;107(1 Suppl):69-74. doi: https://doi.org/10.3171/PED-07/07/069
5. Hamilton SN, Carlson R, Hasan H, et al. Long-term outcomes and complications in pediatric ewing sarcoma. Am J Clin Oncol. 2017;40(4):423-8. doi: https://doi.org/10.1097/COC.0000000000000176
6. Balamuth NJ, Womer RB. Ewing’s sarcoma. Lancet Oncol. 2010;11(2):184-92. doi: https://doi.org/10.1016/S1470-2045(09)70286-4
Recebido em 26/4/2021
Aprovado em 30/8/2021
Scientific Editor: Anke Bergmann. Orcid iD: https://orcid.org/0000-0002-1972-8777
![]()
Este é um artigo publicado em acesso aberto (Open Access) sob a licença Creative Commons Attribution, que permite uso, distribuição e reprodução em qualquer meio, sem restrições, desde que o trabalho original seja corretamente citado.
©2019 Revista Brasileira de Cancerologia | Instituto Nacional de Câncer José Alencar Gomes da Silva | Ministério da Saúde