ARTICLE ORIGINAL
Trends in non-Melanoma
Skin Cancer Mortality in Brazil and its Macroregions
Tendências na Mortalidade
por Câncer de Pele não Melanoma no Brasil e suas Macrorregiões
Tendencias de la Mortalidade por Cáncer de Piel
no Melanoma em Brasil y sus Macrorregiones
doi: https://doi.org/10.32635/2176-9745.RBC.2022v68n1.2083
Maria Isabel do Nascimento1;
Jorge Ricardo Furtado Cardoso de Moraes2; Esther Rohem Costa Silva3;
Maria Gabriela Guinancio da Mota4; Raphael Mendonça Guimarães5
1,2,3,4Universidade
Federal Fluminense (UFF), Faculdade de Medicina. Niterói
(RJ), Brazil. E-mails: maria_isabel@id.uff.br; jorgericardoaz@gmail.com;
esther.rohem@gmail.com; mariaguinancio@id.uff.br. Orcid iD: http://orcid.org/0000-0001-9001-8543;
Orcid iD: http://orcid.org/0000-0003-1731-8720;
Orcid iD: http://orcid.org/0000-0001-7492-5071;
Orcid iD: http://orcid.org/0000-0001-9447-7894
5Fundação
Oswaldo Cruz. Escola Politécnica de Saúde Joaquim Venâncio. Rio de Janeiro
(RJ), Brazil. E-mail: raphael.guimaraes@fiocruz.br. Orcid iD: http://orcid.org/0000-0003-1225-6719
Corresponding
author: Maria Isabel do Nascimento. Hospital
Universitário Antônio Pedro. Secretaria da Coordenação de Medicina. Rua Marquês
do Paraná, 303, 2º andar ‒ Centro. Niterói (RJ), Brazil. CEP
24033-900. E-mail: maria_isabel@id.uff.br
ABSTRACT
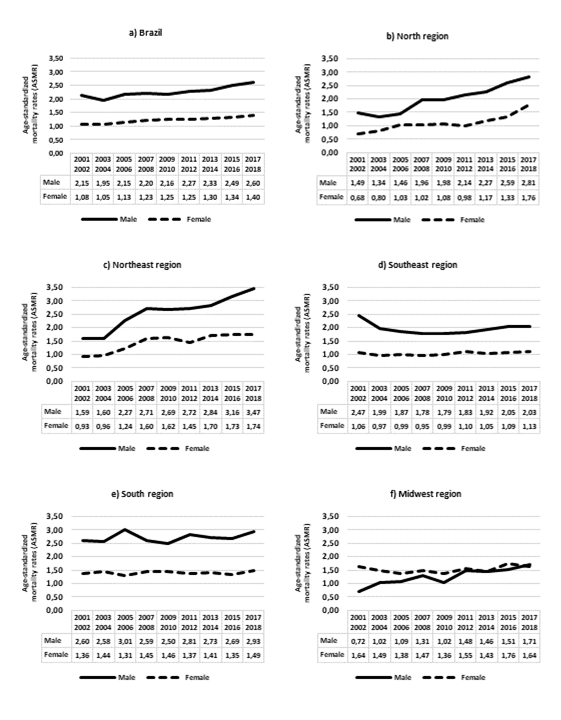
Introduction: Non-melanoma skin cancer (NMSC) is the most
common among all malignancies. Objective:
To describe trends in NMSC mortality rates in Brazil and its macroregions from
2001 to 2018. Method: Adjusted
mortality rates stratified by sex were estimated and presented per 100,000
person-years. An autoregressive analysis was implemented to assess temporal
trends, annual percent change (APC) and 95% Confidence Intervals (95% CI). Results: There were 27,550 NMSC deaths in
Brazil with higher frequency in males (58.1%) and among individuals aged ≥70
years (64.3%). The overall rates were 2.25 (males) and 1.22 (females) per
100,000 person-years. The trends followed an upward direction in Brazil for males
(APC: 2.91%; 95% CI: 1.96%; 3.86%) and females (APC: 3.51%; 95% CI: 2.68%;
4.34%). The same occurred in the North Region, in males (APC: 9.75%; 95% CI:
7.68%; 11.86%) and in females (APC: 10.38; 95% CI: 5.77%; 15.21%), as well as
in Northeast Region, in males (APC: 9.98%; 95% CI: 5.59%; 14.57%) and in females
(APC: 8.34%; 95% CI: 3.29%; 13.64%). Conclusion:
NMSC deaths are not rare in Brazil. Upward mortality trends were observed for
the whole country and in the North and Northeast regions, which are the closest
to the Equator line and also the least developed socioeconomically. A synergism
between different types of inequalities and environmental exposure in these macroregions
may be promoting an increase in the number of NMSC deaths, a type of cancer
which is considered completely preventable.
Key words: skin neoplasms/mortality; time series studies;
developing countries.
RESUMO
Introdução: O câncer de pele não melanoma (CPNM) é o mais comum entre
todas as malignidades. Objetivo:
Descrever as tendências da mortalidade por CPNM no Brasil e nas suas
Macrorregiões, de 2001 a 2018. Método:
As taxas de mortalidade ajustadas por idade e estratificadas por sexo foram
apresentadas por 100 mil pessoas-ano. Uma análise autorregressiva foi implementada
para avaliar tendências, Mudança Percentual Anual (MPA) e intervalos de
confiança de 95% (IC 95%). Resultados:
Houve 27.550 óbitos por CPNM no Brasil com maior frequência em homens (58,1%) e
entre pessoas de 70 anos e mais (64,3%). As taxas globais foram de 2,25
(homens) e 1,22 (mulheres) por 100 mil pessoas-ano. As tendências seguiram em
elevação no Brasil, em homens (MPA: 2,91%; IC95%: 1,96%; 3,86%) e em mulheres
(MPA: 3,51%; IC95%: 2,68%; 4,34%). O mesmo ocorreu na Região Norte, em homens
(MPA: 9,75%; IC95%: 7,68%; 11,86%) e em mulheres (MPA: 10,38%; IC95%: 5,77%;
15,21%), bem como na Região Nordeste, em homens (MPA: 9,98%; IC95%: 5,59%;
14,57%) e em mulheres (MPA: 8,34%; IC95%: 3,29%; 13,64%). Conclusão: Os óbitos por CPNM não são
raridade no Brasil. O país e as Regiões Norte e Nordeste experimentaram taxas
com tendência em elevação. Norte e Nordeste são as Regiões mais próximas da
Linha do Equador e as menos desenvolvidas socioeconomicamente. Nessas Macrorregiões,
um sinergismo entre diferentes tipos de desigualdades e exposições ambientais
pode estar promovendo um aumento dos óbitos por esse tipo de câncer considerado
totalmente evitável.
Palavras-chave: neoplasias cutâneas/mortalidade; estudos de séries
temporais; países em desenvolvimento.
RESUMEN
Introducción: El carcinoma de piel no melanoma (CPNM) es el
más común dentre todas las neoplasias malignas. Objetivo: Describir las tendencias de la mortalidad por CPNM
en Brasil y sus macrorregiones, de 2001 a 2018. Método: Las tasas de mortalidad ajustadas por edad y
estratificadas según sexo fueron presentadas por 100.000 personas-año. Se
implementó una análisis autoregresiva para evaluar las tendencias, el
porcentaje estimado de cambio anual (PECA) y sus intervalos de confianza del
95% (IC 95%). Resultados: Hubo
27.550 muertes por CPNM en Brasil con mayor frecuencia en hombres (58,1%) y
entre personas de edad ≥70 años (64,3%). Las tasas generales fueron 2,25
(hombres) y 1,22 (mujeres) por 100.000 personas-año. Las tendencias continuaron
aumentando en Brasil, en hombres (PECA: 2,91%; IC 95%: 1,96%; 3,86%) y en
mujeres (PECA: 3,51%; IC 95%: 2,68%; 4,34%). Lo mismo ocurrió en el Norte, en
hombres (PECA: 9,75%; IC 95%: 7,68%; 11,86%) y en mujeres (PECA: 10,38%; IC
95%: 5,77%; 15,21%), así como en el Nordeste, en hombres (PECA: 9,98%; IC 95%:
5,59%; 14,57%) y en mujeres (PECA: 8,34%; IC 95%: 3, 29%; 13,64%). Conclusión: Las muertes por CPNM no son una rareza en
Brasil. El país y las regiones Norte y Nordeste experimentaron tasas con
tendencia ascendente. Las regiones Norte y Nordeste son las más cercanas al
Ecuador y también las menos desarrolladas socioeconómicamente. En estas
regiones, una sinergia dentre diferentes tipos de desigualdades y exposiciones
ambientales puede estar promoviendo un aumento de las muertes por este tipo de
cáncer considerado totalmente prevenible.
Palabras
clave: neoplasias
cutáneas/mortalidad; estudios de series temporales; países em desarrollo.
INTRODUCTION
Non-melanoma skin cancer
(NMSC) is a general term used to refer to malignant skin diseases whose origin
is diverse and does not involve melanocytes, as occurs with melanoma skin
cancer (MSC)1. NMSC is the most common cancer type among all the malignancies.
According to the current estimates involving 36 cancer types and 185 countries,
the global occurrence of NMSC reached more than one million new cases in 2018.
The NMSC-related death number worldwide (65,155) was similar to those MSC
(60,712) has caused in the same year2.
The
two major histopathological subtypes under the umbrella of NMSC are Basal Cell
Carcinoma (BCC) and Squamous Cell Carcinoma (SCC); however, if compared to MSC
the epidemiology is understudied3. The most substantial risk factor
for NMSC that epidemiology describes is the exposure to ultraviolet (UV)
radiation4. It is part of the spectrum of electromagnetic radiation
emitted by the sun, and artificial sources, including light bulbs and welding
procedures. UV radiation comprises three wavelength bands (UVA, UVB, and UVC)
that provoke different effects in humans. Potentially, UVA and UVB cause skin
malignancies5.
In
Brazil, estimates of new cancer cases show that the NMSC will be the most
incident in the 2020-2022 triennium, with the annual occurrence of 83,770 (men)
and 93,160 (women) new cases, corresponding to an estimated risk of 80.12 and
86.65 per 100,000 person-year, in men and women, respectively6. In
the rank of all cancer cases in male, in each of the Brazilian macroregions,
the NMSC is the most incident in the South (123.67), Midwest (89.68) and
Southeast (85.55) macroregions, and the second in rank in the Northeast (65.59)
and North (21.28) macroregions. In female, the NMSC occupies the top of rank in
all Brazilian macroregions presenting estimated risk of 125.13 (Midwest),
100.85 (Southeast), 98.49 (South), 63.02 (Northeast), and 39.24 (North) per
100,000 person-year6.
Although
NMSC incidence is high worldwide, studies of mortality are scarce. This
knowledge gap may be explained by the misleading idea that NMSC causes few
deaths, and as a consequence, it is often excluded from large cancer registries
as it creates a barrier for more detailed analysis3. Therefore,
population-based estimates are crucial to scale the true NMSC magnitude and
define the best preventive actions targeting the most vulnerable population
groups7.
In
Brazil, all deaths are regularly registered in the Mortality Information System
managed by the Ministry of Health, specifically, the Department of Informatics
of the National Health System (DATASUS)8. In this context, analyses
of NMSC death data for a continental, tropical country as Brazil can contribute
to improve the understanding of this worldwide public health problem. Thus, the
present study aimed to describe trends in NMSC mortality rates stratified by
sex and age groups in Brazil and its macroregions from the biennium 2001-2002
to 2017-2018.
METHOD
Ecological study conducted in
Brazil with the 2001-2018 nationwide death information from DATASUS8,
which is responsible for managing all vital statistics in Brazil. NMSC death
occurrence was analyzed in the country as a whole as well in five Brazilian macroregions.
Approximately
92% of the Brazilian territory is located in a tropical zone, where 4 of the 5
Brazilian geographic regions (North, Northeast, Southeast, and Midwest) are found.
In Brazil, the UV-radiation level reaches more than 11 points during the summer
solstice9. The World Health Organization (WHO)4 created
the Ultraviolet Index of exposure category, and values from 8 to 10 are
classified as very high, and ≥11, as extreme. It helps to make different
interpretations of UV exposure, potentially harmful to health, regardless of the
type of skin9. The South region, São Paulo state, and part of the
Mato Grosso do Sul state extend throughout the subtropical zone, experiencing
milder temperatures in part of the year.
Number of deaths and population data
The
number of deaths was obtained from the Mortality Information System, a
subsystem coordinated by DATASUS8. This study only included deaths registered
according to code C44 of the International Classification of Diseases – ICD –
10th. revision. Annual population estimates stratified by
demographic characteristics (sex and age) were obtained from the website of “Instituto Brasileiro de Geografia e Estatística”
(IBGE)10.
Mortality rates
Mortality
rates were estimated for eight biennium (from 2001-2002 to 2017-2018) stratified
by sex (male and female) and age groups (30-39, 40-49, 50-59, 60-69, and 70 or
more years). Age-standardized mortality rates (ASMRs) were calculated using the
1960-world population reference11. ASMRs were presented per 100,000
person-year considering Brazil as a whole and its five macroregions.
Trend analysis
At
first, the trend analysis of NMSC mortality in Brazil and in each macroregion was
performed, investigating the ASMR behavior over time displayed in charts. The
dependent variable (ASMR) was plotted in the y-axis and correlated with the
independent variable (biennium) plotted in the x-axis.
Next, a
generalized linear regression was conducted using Prais-Winsten method as
Antunes & Cardoso12 recommend. In this step, Annual Percent
Changes (APC) and respective 95% Confidence Intervals (95% CI) were calculated,
and trends were interpreted as increasing, decreasing, or stable.
Ethical statement
This
study followed the international recommendations and the Brazilian Resolutions of
the National Health Council (CNS) of the Ministry of Health – Resolution number
466/201213 and Resolution number 510/201614 – for
scientific research involving human subjects and as it was developed with de-identified
secondary dataset publicly available on DATASUS website, no IRB (Institutional
Review Board) ethical approval was required.
RESULTS
From 2001 to 2018, 27,550 NMSC
deaths were registered for 30 years-old or older individuals in Brazil. The
frequency of deaths was higher in males (58.1%), among individuals aged ≥70
years (64.3%), and with low (≤4 years) formal education (62.3%). The majority
of deaths occurred with white individuals, both in Brazil and in its macroregions,
except in the North Region where 55.6% of the fatal cases occurred with Brown individuals
(Table 1).
DISCUSSION
This study focused on deaths
attributed to NMSC. It showed that Brazil experienced ASMR higher than 2 per
100,000 person-years in men. Old individuals and men were the most common fatal
victims. These results suggested that mortality rates have increased over time
in the country as a whole, and in the North and the Northeast regions
considering men and women, separately. The most critical variation occurred in
males of the Midwest (139.4%) and in females of the North (158.8%) regions.
This scenario should encourage the implementation of more initiatives to
prevent new deaths and improve the early diagnosis and treatment of NMSC.
Studies
suggest that NMSC frequency maintains an inverse correlation with latitude
variations15. In Brazil, the North and Northeast regions are closer
to the Equator Line than the Southeast, South, and Midwest regions. Besides,
the North region experiences temperatures higher than 18oC through all
months of the year16. However, the most essential question suspected
to be related to upward NMSC mortality is that the North and Northeast regions
are much less developed socioeconomically than the rest of the country. This
condition should be thought as a possible determining factor causing the most
adverse results, mainly considering that the North's and Northeast's population
consists predominantly of Brown and Black individuals, unfortunately having
more restrictive access to high-quality healthcare services. However, this is a
question that demands future investigations and support from policymakers.
Although
in Brazil the lowest incidence rates have been estimated for the North and
Northeast regions6, the current study showed that those two
macroregions have experienced a statistically significant upward mortality
pattern in both sexes, suggesting that the patients may also be facing barriers
to access the health services and to obtain diagnosis and treatment for this
type of cancer. In these regions, there is a great concentration of small
municipalities with rural characteristics and with low demographic density
experiencing unfavorable influences on the implementation of health actions due
to geographical access, precarious living conditions, lack of popular
participation and difficulty in allocating and hiring human resources17.
In this context it is crucial to identify the barriers and propose solutions
capable of changing the disappointing scenario drawn from NMSC mortality in
Brazil and mainly in the North and Northeast regions.
The
protection against skin cancer is highly relevant and recommended for outdoor
workers with occupational sun exposure. In this situation, the risk to develop
skin cancer estimated in meta-analysis was higher than 70% in individuals with
outdoor occupational exposure comparing with workers without sun exposure18.
The most vulnerable occupations are lifeguards, gardeners, fishermen,
construction workers, farmer, rural or agricultural workers19-21.
Agriculture is one of the strongest segments of the Brazilian economy, and
farming workers are particularly important in the North region where livestock
and agriculture play a prominent role in the regional, and family economy22.
Additionally,
leisure activities practiced outdoors also confer an increased risk of NMSC. The use of individual
protection mechanisms should be encouraged during leisure activities and mainly
in the workplace. This involves the use of
appropriate clothing, hats, sunglasses, and sun block products20.
Preventive initiatives should be started in childhood and kept in the daily
routine. However, adherence to preventive recommendations is directly
influenced by socioeconomic conditions, and preventive products may not be
available in the workplace, or people do not have the resources to purchase them
or use them irregularly23. This is another issue that demand more
financial investments and public policy.
Studies
about NMSC deaths have highlighted particular issues. At first, the
disproportionate NMSC mortality observed among African Americans can be related
to the delayed diagnosis and treatment, in part, due to atypical clinical
variations, including lesion appearance and anatomical location in
non-sun-exposed areas24. Another question is that BCC and SCC are
malignancies with distinct behaviors and may be markers of other adverse health
outcomes as all-cause mortality25,26. A Danish cohort study following-up
82,837 patients with BCC and 13,453 with SCC showed excessive death numbers related
to some chronic diseases among patients with SCC but not among patients with
BCC, comparing with the general population27.
A
study with data of the Russian Federation estimated age-standardized mortality
rates of 0.70/100,000 over the 2007-2017 period with a decreasing longitudinal
trend28. However, the majority of the studies about NMSC mortality are
from developed countries. The current results showed age-standardized rates
that are between the values estimated for Australia (around 3.0/100,000) and
Germany (<1.0/100,000) for males, and on the same level for Australia
(around 1.0/100,000), for females7. A common fact occurring in those
countries is the investment in regular public health UV protective practices campaigns
for, and the implementation of body skin cancer screening for insured individuals
aged ≥35, only in Germany7.
Among
the risk factors for NMSC, besides excessive sunlight exposure, increased
longevity, genetic condition, and immune suppression29 are also included.
NMSC is considered rare in children and youngsters. If it occurs with youngsters,
it is suspected to be associated with predisposing heritable and exposure to
iatrogenic risk factors such as prolonged immune suppression, radiation
therapy, chemotherapy and voriconazole use30. Exposed individuals seem
to be at risk of developing skin cancer precociously, and health professionals
other than dermatologists must be involved in the detection of new skin cancer
cases. They will be able to contribute for skin cancer control whether they
were conscious of the extent of the problem, and well-trained to identify any
suspected skin lesions31.
An
important NMSC mortality-related issue is the population ageing observed
worldwide. It is expected that NMSC causes an increasing death number within
the next years given the close relation between keratinocyte cancers and older individuals3.
The effect of UV radiation on the skin is cumulative over time19. Additionally,
immunosenescence is a condition that encourages the development of
opportunistic diseases and malignancies in old age32. Risk factor
exposure over time, and immunosuppressive drug use23 aggravates the
immunosuppressive status. For example, in a cohort of 165 patients with renal
transplantation and at least one year of follow-up at a Brazilian reference
center33, 19 NMSC in eleven of them (6.67%) were found.
This study
has advantages and limitations. Firstly, an advantage results from the fact that
investigations using NMSC mortality data are still scarce both in Brazil and
worldwide. Thus, the study contributed to improve the understanding of this
problem in developing countries, since NMSC has been suspected to be increasing
in some countries. For example, excluding low risk individuals who are
foreigners from Asia, the Pacific Islands, the Middle East, and sub-Saharan
Africa, as well as Australian aborigines and Maori from New Zealand, NMSC
deaths increased 208% in Australia, between 1981 and 2011, with figures rising
7% a year34. Another contribution was estimating age-standardized
rates using as reference the 1960-world standardized population designated by
Segi et al.11. Thus, the standardization procedure may have made the
current results more adequate for future international comparisons. However,
this routine-data-based study presents some limitations, such as missing values
of skin color and education variables. Even though they have been used only to
describe the population characteristics briefly, it is a problem that needs to
be pointed out. Another question is that the use of aggregated data prevents
the result extrapolation for the individual level. However, it is possible that
these results have provided useful background that may help to address the
decisions against NMSC mortality.
CONCLUSION
In
summary, NMSC deaths are not rare in Brazil. The country as a whole, and the
North and Northeast regions have experienced upward mortality trends. The North
and Northeast regions are the closest to the Equator Line and are also the
least developed socioeconomically. In these macroregions, a synergism between
different types of inequalities and environmental exposure may be promoting an
increase in the number of NMSC deaths, a type of cancer which is considered
completely preventable.
CONTRIBUTIONS
Maria
Isabel do Nascimento, Jorge Ricardo Furtado Cardoso de Moraes, Esther Rohem
Costa Silva, Maria Gabriela Guinancio da Mota contributed equally to
conceptualization, study planning, data collecting, formal statistics analysis,
interpretation of the results and original drafting. Raphael Mendonça Guimarães
participed in the phases of analysis and interpretation of the results and
critically reviewed the manuscript. All authors reviewed and approved this
version and are responsible for the accuracy and integrity of the work.
CONFLICT OF INTEREST
The
authors have no conflicts of interest to declare.
FUNDING
FAPERJ
for scientific initiation scholarship number 200.418/2019.
REFERENCES
1. Liu-Smith F, Jia J, Zheng Y. UV-induced
molecular signaling differences in melanoma and non-melanoma skin cancer. Adv
Exp Med Biol 2017;996:27-40. doi: https://doi.org/10.1007/978-3-319-56017-5_3
2. Bray F, Ferlay J, Soerjomataram I, et al. Global
cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide
for 36 cancers in 185 countries. Ca
Cancer J Clin. 2018;68:394-424. doi: https://doi.org/10.3322/caac.21492
3.
Apalla Z, Lallas A, Sotiriou E, et al. Epidemiological
trends in skin cancer. Dermatol Pract Concept. 2017;7(2):1-6. doi: https://doi.org/10.5826/dpc.0702a01
4. World Health Organization, World
Meteorological Organization, United Nations Environment Programme,
International Commission on Non-Ionizing Radiation Protection. Global Solar UV
index: a practical guide [Internet]. Geneva: WHO; 2002 [cited 2020 June 10].
Available from: https://apps.who.int/iris/handle/10665/42459
5. Paulo MS, Adam B, Akagwu C, et al. WHO/ILO
work-related burden of disease and injury: protocol for systematic reviews of
occupational exposure to solar ultraviolet radiation and of the effect of
occupational exposure to solar ultraviolet radiation on melanoma and non-melanoma
skin cancer. Environ Int. 2019;126:804-15. doi:
https://doi.org/10.1016/j.envint.2018.09.039
6.
Instituto Nacional de Câncer José Alencar Gomes da Silva. Estimativa 2020:
incidência de câncer no Brasil [Internet]. Rio de Janeiro: INCA; 2019 [acesso
2020 jun 15]. Disponível em: https://www.inca.gov.br/publicacoes/livros/estimativa-2020-incidencia-de-cancer-no-brasil
7. Stang A, Khil L, Kajüter H, et al. Incidence
and mortality for cutaneous squamous cell carcinoma: comparison across three
continents. J Eur Acad Dermatol Venereol.
2019;33(Suppl 8):6-10. doi: https://doi.org/10.1111/jdv.15967
8.
Ministério da Saúde (BR), Departamento de Informática do SUS. DATASUS:
informações de saúde (TABNET) [Internet]. Brasília, DF: DATASUS; c2008 [acesso
2020 maio 22]. Disponível em: http://www2.datasus.gov.br/DATASUS/index.php
9.
Corrêa MP. Solar
ultraviolet radiation: properties, characteristics and amounts observed in
Brazil and South America. An
Bras Dermatol. 2015;90(3):297-313. doi: https://doi.org/10.1590/abd1806-4841.20154089
10.
Instituto Brasileiro de Geografia e Estatística. Estatísticas [Internet]. Rio
de Janeiro: IBGE; c2020. Projeções da população: o que é; [acesso 2020 jun 23].
Disponível em: https://www.ibge.gov.br/estatisticas/sociais/populacao/9109-projecao-da-populacao.html?=&t=o-que-e
11. Segi M, Kurihara M, Matsuyama T. Cancer
mortality for selected sites in 24 countries No. 5 (1964-1965). Sendai, Japan:
Tohoku University School of Medicine; 1969.
12. Antunes JLF, Cardoso MRA. Uso da análise de séries temporais em estudos
epidemiológicos. Epidemiol Serv Saúde. 2015;24(3):565-76. doi: https://doi.org/10.5123/S1679-49742015000300024
13.
Conselho Nacional de Saúde (BR). Resolução nº 466, de 12 de dezembro de 2012.
Aprova as diretrizes e normas regulamentadoras de pesquisas envolvendo seres
humanos. Diário Oficial da União, Brasília, DF. 2013 jun 13; Seção 1:59.
14.
Conselho Nacional de Saúde (BR). Resolução nº 510, de 7 de abril de 2016.
Dispõe sobre as normas aplicáveis a pesquisas em Ciências Humanas e Sociais
cujos procedimentos metodológicos envolvam a utilização de dados diretamente
obtidos com os participantes ou de informações identificáveis ou que possam
acarretar riscos maiores do que os existentes na vida cotidiana, na forma
definida nesta Resolução. Diário Oficial da União. 2016 maio 24; Edição98,
Seção I:44.
15.
Rivas M, Rojas E, Calaf GM, et al. Association
between non-melanoma and melanoma skin cancer rates, vitamin D and latitude. Oncol Lett. 2017;13(5):3787-92. doi: https://doi.org/10.3892/ol.2017.5898
16.
Instituto Brasileiro de Geografia e Estatística [Internet]. Rio de Janeiro:
IBGE; c2020. Clima: 2002 clima: 1:5 000 000: mapa de clima do Brasil; [acesso 2021
jan 3]. Disponível em: https://www.ibge.gov.br/geociencias/informacoes-ambientais/climatologia/15817-clima.html?=&t=downloadschrome-
17. Calvo MCM, Lacerda JT, Colussi CF, et al. Municipalities stratification for health
performance evaluation. Epidemiol Serv Saude. 2016;25(4):767-76. doi: https://doi.org/10.5123/s1679-49742016000400010
18. Schmitt J, Seidler A, Diepgen TL, et al.
Occupational ultraviolet light exposure increases the risk for the development
of cutaneous squamous cell carcinoma: a systematic review and meta-analysis. Br
J Dermatol. 2011;164(2):291-307. doi: https://doi.org/10.1111/j.1365-2133.2010.10118.x
19. Modenese A, Korpinen L, Gobba F. Solar
radiation exposure and outdoor work: an underestimated occupational risk. Int J
Environ Res Public Health. 2018;15(10):2063. doi: https://doi.org/10.3390/ijerph15102063
20.
Instituto Nacional de Câncer José Alencar Gomes da Silva. Diretrizes para a
vigilância do câncer relacionado ao trabalho [Internet]. 2. ed. rev. e atual.
Rio de Janeiro: INCA; 2013 [acesso 2021 ago 20]. Disponível em: https://www.inca.gov.br/publicacoes/livros/diretrizes-para-vigilancia-do-cancer-relacionado-ao-trabalho
21.
Ceballos AGC, Santos SL, Silva ACA, et al. Exposição solar ocupacional e câncer
de pele não melanoma: estudo de revisão integrativa. Rev Bras Cancerol.
2014;60(3):251-8. doi: https://doi.org/10.32635/2176-9745.RBC.2014v60n3.472
22.
Castro CN. A agropecuária na região Norte: oportunidades e limitações ao
desenvolvimento. Texto para discussão. Brasília, DF; Rio de Janeiro: IPEA; 2013
[acesso 2021 ago 22]. (Texto para discussão; 1836). Disponível em: http://repositorio.ipea.gov.br/bitstream/11058/1215/1/TD_1836.pdf
23.
Imanichi D, Gasparello Filho JL, Moraes CF, et al. Fatores de risco do câncer
de pele não melanoma em idosos no Brasil. Diagn Tratamento. 2017;22(1):3-7.
24.
Higgins S, Nazemi A, Chow M, et al. Review
of nonmelanoma skin cancer in African Americans, Hispanics, and Asians. Dermatol
Surg. 2018;44(7):903-10. doi: https://doi.org/10.1097/dss.0000000000001547
25. Wehner MR, Cidre Serrano W, Nosrati A, et
al. All-cause mortality in patients with basal and squamous cell carcinoma: a
systematic review and meta-analysis. J Am Acad Dermatol. 2018;78(4):663-72. doi:
https://doi.org/10.1016/j.jaad.2017.11.026
26. Barton V, Armeson K, Hampras S, et al.
Nonmelanoma skin cancer and risk of all-cause and cancer-related mortality: a
systematic review. Arch Dermatol Res. 2017;309(4):243-51. doi: https://doi.org/10.1007/s00403-017-1724-5
27. Jensen AØ, Bautz A, Olesen AB, et al. Mortality
in Danish patients with nonmelanoma skin cancer, 1978-2001. Br J Dermatol. 2008;159(2):419-25. doi: https://doi.org/10.1111/j.1365-2133.2008.08698.x
28.
Muntyanu A, Ghazawi FM, Nedjar H, et al. Non-melanoma
skin cancer distribution in the Russian Federation. Dermatol. 2021;237(6):1007-15.
doi: https://doi.org/10.1159/000512454
29. Leiter U, Garbe C. Epidemiology of melanoma
and nonmelanoma skin cancer - the role of sunlight. Adv Exp Med Biol.
2008;624:89-103. doi: https://doi.org/10.1007/978-0-387-77574-6_8
30. Khosravi H, Schmidt B, Huang JT.
Characteristics and outcomes of nonmelanoma skin cancer (NMSC) in children and
young adults. J Am Acad Dermatol. 2015;73(5):785-90. doi: https://doi.org/10.1016/j.jaad.2015.08.007
31. Leiter U, Keim U, Eigentler T, et al. Incidence, mortality, and trends of nonmelanoma
skin cancer in Germany. J Invest Dermatol. 2017;137(9):1860-67. doi: https://doi.org/10.1016/j.jid.2017.04.020
32. Perrotta RE, Giordano M, Malaguarnera M. Non-melanoma
skin cancers in elderly patients. Crit Rev Oncol Hematol. 2011;80(3):474-80.
doi: https://doi.org/10.1016/j.critrevonc.2011.04.011
33. Gonçalves CP, Trope BM, Ramos-e-Silva M. Non-melanoma
skin cancer in renal transplant recipients: a study in a Brazilian reference
center. Clin Cosmet Investig Dermatol. 2015;8:339-44. doi: https://doi.org/10.2147/CCID.S78456
34. Czarnecki D. Non-melanoma skin cancer
mortality rising in susceptible Australians [letters]. J Eur Acad Dermatol Venereol. 2017;31(6):e286-e7. doi: https://doi.org/10.1111/jdv.14052
Recebido
em 31/5/2021
Aprovado
em 13/10/2021
Associate Editor: Jeane
Tomazelli. Orcid iD: https://orcid.org/0000-0002-2472-3444
Scientific
Editor: Anke Bergmann. Orcid iD: https://orcid.org/0000-0002-1972-8777

Este é um artigo
publicado em acesso aberto (Open Access) sob a licença Creative Commons
Attribution, que permite uso, distribuição e reprodução em qualquer meio, sem
restrições, desde que o trabalho original seja corretamente citado.
©2019 Revista
Brasileira de Cancerologia | Instituto Nacional de Câncer José Alencar Gomes da
Silva | Ministério da Saúde