CASE REPORT
Pulmonary Benign Metastasizing Leiomyoma: Case Report of Late Occurrence in Postmenopausal Patient
Leiomiomatose Benigna Metastatizante Pulmonar: Relato de um Caso com Ocorrência Tardia em Paciente Pós-menopausa
Leiomiomatosis Benigna Metastatizante Pulmonar: Reporte de un Caso con Ocurrencia Tardía en Paciente Posmenopáusica
doi: https://doi.org/10.32635/2176-9745.RBC.2022v68n1.2408
Rafael Everton Assunção Ribeiro da Costa1; Lina Gomes dos Santos2; Julio Benevides Viana Neves3; Cristiane Amaral dos Reis4
1Centro de Ciências da Saúde, Universidade Estadual do Piauí. Teresina (PI), Brazil. E-mail: rafaelearcosta@gmail.com. Orcid iD: https://orcid.org/0000-0002-0798-890X
2,3Hospital São Marcos. Teresina (PI), Brazil. E-mail: linagsantos@gmail.com; jbvneves@hotmail.com. Orcid iD: https://orcid.org/0000-0001-6345-928X; Orcid iD: https://orcid.org/0000-0002-8900-9655
4Oncocenter. Teresina (PI), Brazil. E-mail: amaraldosreis@yahoo.com.br. Orcid iD: https://orcid.org/0000-0002-3807-3382
Corresponding author: Rafael Everton Assunção Ribeiro da Costa. Rua Olavo Bilac, 2335 – Centro. Teresina (PI), Brazil. CEP 64001-280. E-mail: rafaelearcosta@gmail.com
ABSTRACT
Introduction: Pulmonary benign metastasizing leiomyoma (PBML) is a rare condition that occurs most commonly in young women of reproductive age some years after hysterectomy. The aim of this study was to report a PBML case which occurred 33 years after hysterectomy in a postmenopausal patient. Case report: A 59-year-old female diabetic patient, G2P2A0, with dyslipidemia, a non-smoker and ex-alcoholic (quit in the 90s), with pulmonary symptoms was referred to the health service. A chest computed tomography (CT) revealed multiple pulmonary nodules. A previous history of hysterectomy at 26 years of age led to a diagnostic hypothesis of PBML. The patient underwent segmentectomy of the largest nodule (measuring 1.2 x 0.9 cm) located in the left lung. Histopathology and immunohistochemistry studies confirmed the diagnosis of PBML. Conclusion: The patient is currently in good physical condition (regression of previous pulmonary symptoms) and scheduled for clinical follow-up. A new chest CT will be performed in 6 months.
Key words: leiomyomatosis; uterine neoplasms; lung neoplasms; neoplasm metastasis; case reports.
RESUMO
Introdução: A leiomiomatose benigna metastatizante pulmonar (LBMP) é uma doença rara, ocorrendo mais comumente em mulheres jovens em idade reprodutiva alguns anos após a realização de histerectomia. O objetivo deste estudo foi relatar um caso de LBMP de ocorrência tardia, 33 anos após a realização de histerectomia, em uma paciente pós-menopausa. Relato do caso: Paciente do gênero feminino, 59 anos, G2P2A0, diabética, dislipidêmica, não tabagista e ex-etilista (parou na década de 1990), foi encaminhada ao serviço médico com sintomas pulmonares, sendo realizada tomografia computadorizada (TC) de tórax que revelou múltiplos nódulos pulmonares. Havia história prévia de histerectomia aos 26 anos de idade, sendo levantada a hipótese diagnóstica de LBMP. Paciente realizou segmentectomia do maior nódulo (medindo 1,2 x 0,9 cm) localizado no pulmão esquerdo. Exame anatomopatológico e imuno-histoquímica confirmaram o diagnóstico de LBMP. Conclusão: Atualmente, a paciente se encontra em seguimento clínico e em bom estado geral (sem os sintomas pulmonares apresentados inicialmente). Será realizada uma nova TC de tórax em seis meses.
Palavras-chave: leiomiomatose; neoplasias uterinas; neoplasias pulmonares; metástase neoplásica; relatos de casos.
RESUMEN
Introducción: La leiomiomatosis benigna metastatizante pulmonar (LBMP) es una enfermedad rara, que ocurre con mayor frecuencia en mujeres jóvenes en edad reproductiva pocos años después de la histerectomía. El objetivo de este estudio fue reportar un caso de LBMP de inicio tardío, 33 años después de la histerectomía, en una paciente posmenopáusica. Reporte del caso: Paciente de género femenino, 59 años, G2P2A0, diabética, dislipidémica, no fumadora y exalcohólica (parado en los 90), fue remitida al servicio por cuadro pulmonar, siendo sometida a tomografía computarizada (TC) de tórax, que reveló múltiples nódulos pulmonares. Existía antecedente de histerectomía a los 26 años, planteando la hipótesis diagnóstica de LBMP. Paciente fue sometida a segmentectomía del nódulo de mayor tamaño (de 1,2 x 0,9 cm) localizado en el pulmón izquierdo. El examen patológico y la inmunohistoquímica confirmaron el diagnóstico de LBMP. Conclusión: Actualmente la paciente se encuentra en seguimiento clínico y en buen estado general (sin los síntomas pulmonares presentados inicialmente). Se realizará una nueva TC de tórax en seis meses.
Palabras clave: leiomiomatosis; neoplasias uterinas; neoplasias pulmonares; metástasis de la neoplasia; informes de casos.
INTRODUCTION
Benign metastasizing leiomyoma (BLM) is a rare disorder that affects primarily the lungs and occurs most commonly in young women of reproductive age. Pulmonary BLM (PBML) is characterized by the presence of multiple small pulmonary nodules, usually detectable by imaging tests many years (generally up to 20 years) after hysterectomy. Definitive diagnosis is made by histopathology and immunohistochemistry studies of leiomyoma in the pulmonary lesions1,2.
The aim of this study is to report the late occurrence of PBML in a postmenopausal woman 33 years after she underwent hysterectomy.
CASE REPORT
A 59-year-old female diabetic patient, G2P2A0, with dyslipidemia, a non-smoker and ex-alcoholic (quit in the 90s), was referred to the health service in May 2021. She had a family history of breast and uterine cancer. In mid- 2020, the patient presented with asthenia, intermittent nonproductive cough, occasionally with mucus secretion, headache, and suspicion of fever (without a thermometer). The patient denied hyporexia and weight loss. She complained of intermittent progressive dorsal pain, alleviated by the use of nonsteroidal anti-inflammatory drugs, and also described episodes of epigastric pain.
A chest computed tomography (CT scan) showed bilateral apical pleural thickening with the presence of multiple solid pulmonary nodules. Nodules were well- demarcated and diffuse, and the largest lesion measured 1.2 x 0.9 cm (Figure 1). There were no enlarged mediastinal lymph nodes. The patient had undergone hysterectomy at 26 years of age, and the diagnostic hypothesis was PBML.
|
|
|
Figure 1. Lung nodules of pulmonary benign metastasizing leiomyoma on chest CT-scan |
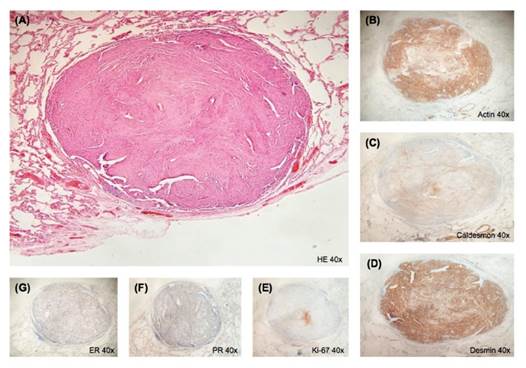
Due to the presence of multiple small nodules scattered throughout the lungs, the thoracic surgeons chose to perform segmentectomy of the largest node in the left lung in August 2021. The surgical specimen was sent to the laboratory for histopathology and immunohistochemistry studies (Figure 2).
|
|
|
Figure
2.
(A): Histopathology (Hematoxylin-Eosin – HE). (B): Actin. |
Histopathology and immunohistochemistry studies described a well-demarcated lesion in the pulmonary parenchyma consisting of the proliferation of elongated spindle-shaped cells arranged in short and/or intertwined bundles, sometimes exhibiting imprisoned mature respiratory epithelium. There were no mitotic figures, atypias and/or necrosis. Neoplastic cells expressed muscle actin, desmin and caldesmon, along with a low Ki-67 proliferation index (Ki-67 < 5%) and diffuse positivity for hormone receptors (ER/PR). A diagnosis of PBML was confirmed by morphologic and immunophenotypical findings and based on the patient’s history of hysterectomy due to uterine leiomyoma. After surgery, the patient remains in good physical condition (regression of previous pulmonary symptoms). Clinical follow-up was scheduled to take place in 6 months with a new CT scan.
This study is part of a project with oncology patients treated in a private Oncology Center located in the city of Teresina (Piauí - PI), Brazil. The Institutional Review Board of the State University of Piauí, Teresina (PI), Brazil approved the project (CAAE: 30154720.0.0000.5209), having complied with the ethical principles of Resolution 466/123 of the Brazil’s National Health Council and international norms. The patient signed the informed consent form (ICF).
DISCUSSION
PBML is a rare condition, with around 160 cases reported to date in the literature4. Its cause remains uncertain. Studies in the literature attribute three main hypotheses for the occurrence of PBML: (1): transportation of smooth muscle cells through blood and lymph vessels to the lungs and other sites after myomectomy or hysterectomy (transport theory – main hypothesis); (2): metastatic pulmonary nodules of PBML are actually malignant, highly differentiated, low-grade leiomyosarcomas; and (3): the origin of PBML is multifocal, since some cases were detected before or simultaneously with uterine leiomyomas. Therefore, pulmonary nodules in PBML would be considered multiple smooth muscle hamartomas and not metastases5.
PBML is more common in young women of reproductive age, and mean age at diagnosis is 47.3 years. Clinical course of the disease is related to reproductive hormone levels. Mean age at detection of PBML after hysterectomy is 8.8 years. It is usually an asymptomatic and incidental finding in chest imaging tests. However, about 30% of patients have pulmonary symptoms (shortness of breath, coughing and chest pain, among others)4-7.
A series of events occurred that are uncommon to PBML. First, the disease was detected at an advanced age (59 years) in the postmenopausal period, which is unusual. It was also included in the smallest percent of patients with pulmonary symptoms. Furthermore, a prolonged time period elapsed between the hysterectomy and the emergence of nodules (around 33 years).
A chest CT scan is the preferential diagnostic imaging method to investigate the pulmonary nodules in PBML. Histopathology and immunohistochemistry studies provide the definitive diagnosis. Due to poor understanding of PBML, there is still no standard treatment. Fan et al. published a series of 23 PBML cases in 2020, and to date it is the study with the largest number of PBML cases. In their study, these authors showed that in patients with pulmonary nodules limited to a certain pulmonary region or a single nodule, curative surgeries for the removal of pulmonary nodules produce good clinical outcomes8,9. The patient had multiple small nodules scattered throughout the lungs. The thoracic surgeons chose to perform segmentectomy of the largest nodule located in the left lung and regression of initial pulmonary symptoms occurred.
CONCLUSION
The patient is undergoing clinical follow-up and remains in good physical condition, with no pulmonary symptoms. A new chest CT will be performed in 6 months.
CONTRIBUTIONS
Rafael Everton Assunção Ribeiro da Costa: Study design, data acquisition, quality control of data, data analysis and interpretation, wording and review. Lina Gomes dos Santos: Study design, data acquisition, quality control, analysis and interpretation of the data and wording. Julio Benevides Viana Neves: Study design, acquisition, quality control, analysis and interpretation of the data and wording. Cristiane Amaral dos Reis: Study design, acquisition, quality control, analysis and interpretation of the data, wording, and critical review. All the authors approved the final version to be published.
DECLARATION OF CONFLICT OF INTERESTS
There is no conflict of interests to declare.
FUNDING SOURCES
None.
REFERENCES
1. Fatima S, Ahmed Z, Azam M. Benign metastasizing leiomyoma. Indian J Pathol Microbiol. 2010;53(4):802- 4. doi: https://doi.org/10.4103/0377-4929.72099
2. Nuovo GJ, Schmittgen TD. Benign metastasizing leiomyoma of the lung: clinicopathologic, immunohistochemical, and micro-RNA analyses. Diagn Mol Pathol. 2008;17(3):145-50. doi: https://doi. org/10.1097/PDM.0b013e31815aca19
3. Conselho Nacional de Saúde (BR). Resolução nº 466, de 12 de dezembro de 2012. Aprova as diretrizes e normas regulamentadoras de pesquisas envolvendo seres humanos. Diário Oficial da União, Brasília, DF. 2013 jun 13; Seção 1:59.
4. Jo HC, Baek JC. Case of pulmonary benign metastasizing leiomyoma from synchronous uterine leiomyoma in a postmenopausal woman. Gynecol Oncol Rep. 2018;26:33-6. doi: https://doi.org/10.1016/j. gore.2018.08.009
5. Dai HY, Guo SL, Shen J, et al. Pulmonary benign metastasizing leiomyoma: a case report and review of the literature. World J Clin Cases. 2020;8(14):3082-9. doi: https://doi.org/10.12998/wjcc.v8.i14.3082
6. Raposo MI, Meireles C, Cardoso M, et al. Benign metastasizing leiomyoma of the uterus: rare manifestation of a frequent pathology. Case Rep Obstet Gynecol. 2018;2018:5067276. doi: https://doi. org/10.1155/2018/5067276
7. Jiang H, Ma L, Qi XW, et al. Pulmonary benign metastasizing leiomyoma: a case report and literature review. Ann Palliat Med. 2021;10(5):5831-8. doi: https://doi.org/10.21037/apm-20-878
8. Choe YH, Jeon SY, Lee YC, et al. Benign metastasizing leiomyoma presenting as multiple cystic pulmonary nodules: a case report. BMC Womens Health. 2017;17:81. doi: https://doi.org/10.1186/s12905-017- 0435-6
9. Fan R, Feng F, Yang H, et al. Pulmonary benign metastasizing leiomyomas: a case series of 23 patients at a single facility. BMC Pulm Med. 2020;20(1):292. doi: https://doi.org/10.1186/s12890-020-01330-4
Recebido em 14/10/2021
Aprovado em 3/12/2021
Scientific-Editor: Anke Bergmann. Orcid iD: https://orcid.org/0000-0002-1972-8777
![]()
Este é um artigo publicado em acesso aberto (Open Access) sob a licença Creative Commons Attribution, que permite uso, distribuição e reprodução em qualquer meio, sem restrições, desde que o trabalho original seja corretamente citado.
©2019 Revista Brasileira de Cancerologia | Instituto Nacional de Câncer José Alencar Gomes da Silva | Ministério da Saúde