ORIGINAL ARTICLE
Quality of Life of Chilean Breast Cancer Survivors: Multicentric Study
Qualidade de Vida de Sobreviventes de Câncer de Mama do Chile: Estudo Multicêntrico
Calidad de Vida de Sobrevivientes de Cáncer de Mama de Chile: Estudio Multicentrico
doi: https://doi.org/10.32635/2176-9745.RBC.2023v69n1.2757
1Hospital del Salvador, Servicio de Medicina Física y Rehabilitación. Santiago de Chile, Chile. E-mail: alejandralorcap@gmail.com. Orcid iD: https://orcid.org/0000-0001-6832-7315
2Facultad de Medicina, Clínica Alemana Universidad del Desarrollo. Santiago de Chile, Chile. E-mail: csacomori@yahoo.com.br. Orcid iD: https://orcid.org/0000-0002-7349-7850
3Hospital de Quilpué, Unidad de Kinesiología, Quilpué, Chile. Universidad Santo Tomás, Facultad de Salud, Escuela de Kinesiología. Viña del Mar, Chile. E-mail: sandra.kines2@gmail.com. Orcid iD: https://orcid.org/0000-0002-8859-5752
4Complejo Asistencial Dr. Victor Ríos Ruiz, Centro de Costo Medicina Física y Rehabilitación. Los Angeles, Chile. E-mail: aliciahinrichsen@gmail.com. Orcid iD: https://orcid.org/0000-0001-6235-577X
5,6,7Hospital del Salvador. Santiago de Chile, Chile. E-mails: khla.lopez@gmail.com; mvegaosorio@gmail.com; pcontalba@hsalvador.cl. Orcid iD: https://orcid.org/0000-0001-9420-5047; Orcid iD: https://orcid.org/0000-0002-4494-0307; Orcid iD: https://orcid.org/0000-0002-2774-593X
8Universidade do Estado de Santa Catarina, Departamento de Fisioterapia. Florianópolis (SC), Brazil. E-mail: fabiana.sperandio@udesc.br. Orcid iD: https://orcid.org/0000-0002-2435-0246
Corresponding author: Cinara Sacomori. Avenida Plaza 680, Las Condes. Santiago, Chile. E-mail: csacomori@yahoo.com.br
ABSTRACT
Introduction: As breast cancer survivorship rates increase, so does the necessity to improve survivors’ health-related quality of life (HRQoL). Objective: To analyze HRQoL among Chilean breast cancer survivors, in general and considering geographic location. In addition, to correlate HRQoL with age, education level and body mass index (BMI). Method: Cross-sectional observational study which included 125 female breast cancer survivors from three public hospitals in three Chilean Macroregions: Central, North Central, and South. The EORTC Questionnaires, QLQ-C30 and QLQ-BR23, and sociodemographic and clinical records were applied. Results: The mean age was 56.1 (±11.9) years with a HRQoL summary score of 67.6 (21.9). HRQoL was reduced mainly in emotional functioning, pain, and insomnia. Fatigue, dyspnea, appetite loss, constipation, financial difficulties, breast and arm symptoms were also reported. The women from the South Macroregion Hospital presented the worst HRQoL scores for most of the domains [general health, functioning (physical, emotional, cognitive and social), fatigue, and nausea], p<0.001. The summary score of HRQoL was correlated to age (Spearman´s rho=0.202, p=0.033), BMI (rho=-0.341, p<0.001), and education level (rho=0.310, p=0.001). Conclusion: Women from three Macroregions showed differences in HRQoL. The latter correlated to age, BMI, and education level. Considering the high presence of symptoms, it is necessary to improve survivorship care plans, providing access to rehabilitation in the continuum of care.
Key words: breast neoplasms; quality of life; social determinants of health; cancer survivors; health promotion.
RESUMO
Introdução: À medida que as taxas de sobrevivência do câncer de mama aumentam, também aumenta a necessidade de melhorar a qualidade de vida relacionada à saúde (QVRS) dos sobreviventes. Objetivo: Analisar a QVRS em geral e considerando a localização geográfica entre sobreviventes de câncer de mama chilenas. Além disso, correlacionar a QVRS com idade, nível educacional e índice de massa corporal (IMC). Método: Estudo observacional transversal que incluiu 125 mulheres sobreviventes de câncer de mama de três hospitais públicos em três Macrorregiões chilenas: Central, Norte-Central e Sul. Foram utilizados os Questionários EORTC QLQ-C30 e QLQ-BR23 e os registros sociodemográficos e clínicos. Resultado: A média de idade foi de 56,1 (±11,9) anos com escore resumido de QVRS de 67,6 (21,9). A QVRS estava reduzida principalmente no funcionamento emocional, dor e insônia. Fadiga, dispneia, perda de apetite, constipação, dificuldades financeiras, sintomas de braço e mama também foram mencionados. As mulheres do hospital da Macrorregião Sul apresentaram os piores escores de QVRS para a maioria dos domínios [saúde geral, funcionamento (físico, emocional, cognitivo e social), fadiga e náusea], p<0,001. A pontuação geral de QVRS esteve correlacionada com idade (rho de Spearman=0,202, p=0,033), IMC (rho=-0,341, p<0,001) e nível educacional (rho=0,310, p=0,001). Conclusão: As mulheres das três Macrorregiões apresentaram diferenças na QVRS. Esta última se correlacionou com idade, IMC e nível educacional. Considerando a alta presença de sintomas, há necessidade de aprimoramento dos planos de atenção à sobrevivência, possibilitando acesso à reabilitação no contínuo do cuidado.
Palavras-chave: neoplasias da mama; qualidade de vida; determinantes sociais da saúde; sobreviventes de câncer; promoção da saúde.
RESUMEN
Introducción: A medida que aumentan las tasas de supervivencia al cáncer de mama, también aumenta la necesidad de mejorar la calidad de vida relacionada con la salud (CdV) de las sobrevivientes. Objetivo: Analizar la CdV entre supervivientes chilenas de cáncer de mama, en general y considerando ubicación geográfica. Además, correlacionar CdV con edad, nivel educacional e índice de masa corporal (IMC). Método: Estudio observacional transversal que incluyó a 125 mujeres sobrevivientes de cáncer de mama de tres Hospitales públicos de tres Macrorregiones de Chile: Centro, Centro Norte y Sur. Se utilizaron los Cuestionarios EORTC QLQ-C30 y QLQ-BR23, historias sociodemográficas y clínicas. Resultados: La edad media fue de 56,1 (±11,9) años con una puntuación resumida de CdV de 67,6 (21,9). La CdV estuvo disminuida principalmente en funcionamiento emocional, dolor e insomnio. Fatiga, disnea, pérdida de apetito, estreñimiento, dificultades financieras, síntomas de brazo y mama también fueron reportados. Las mujeres del hospital de la Macrorregión Sur presentaron las peores puntuaciones de calidad de vida en la mayoría de los dominios [salud general, funcionamiento (físico, emocional, cognitivo y social), fatiga y nausea], p<0,001. El puntaje de CdV estuvo correlacionado con edad (rho de Spearman =0,202, p=0,033), IMC (rho=-0,341, p<0,001) y nivel educacional (rho=0,310, p=0,001). Conclusión: Las mujeres pertenecientes a tres regiones presentaron diferencias en la CdV. Esta última se correlacionó con edad, IMC y nivel educacional. Considerando la elevada presencia de síntomas, es necesario mejorar los planes de atención a las sobrevivientes, posibilitando acceso a rehabilitación en el continuo de los cuidados.
Palabras clave: neoplasias de la mama; calidad de vida; determinantes sociales de la salud; supervivientes de cáncer; promoción de la salud.
INTRODUCTION
Breast cancer is the most commonly diagnosed malignancy and the primary cause of death by cancer among women worldwide1. By 2050, nearly 3.2 million new cases are expected annually in the whole world2. In Chile, breast cancer is very incident with higher mortality rates and its diagnosis and treatment is of universal access since 20053.
With survivorship increase after diagnosis and treatments, changes in post-illness quality of life are now of great interest4,5. Health-related quality of life (HRQoL) is generally accepted as a multidimensional assessment of how disease and treatment affect a patient’s sense of overall function and wellbeing in their physical, psychological, and social dimensions6. More recently, new conceptual approaches were addressed within the concept of HRQoL, incorporating contextual components related to the cultural, political, social, economic, and ecological environments7.
HRQoL is influenced by contextual factors, such as treatment regimens and patients’ perceptions about breast cancer8, more advanced tumor stage4,5, more comorbidities4, receiving chemotherapy8, pain, low cognitive function5, and obesity9. There is evidence that pain is reported by 25-60% of breast cancer surviving patients associated with clinical and surgical aspects10. Socioeconomic variables also interfere in this context2,7. Accordingly, a meta-analysis concluded that regional differences affect cancer outcomes, for example, women living in rural areas were more likely than urban women to be diagnosed at an advanced stage disease, predicting worse HRQoL11. In Brazil, recent data showed that compliance with recommendations for early diagnosis of breast cancer is not the same across the country regions12. A metanalysis with Latin America and Caribbean breast cancer survivors indicated that HRQoL domain scores differ between countries and stage cancer survivors13. The latter found more information from Brazil, Mexico, and Colombia13.
Considering that HRQoL is the result of a good balance between physical, mental and social aspects6,7, it was reasonable to carry out an exploratory study, unprecedented in Chile, in order to map different geographical contexts. This research may give voice to the future clinical management of these women, since the increasing industrialization and the effective presence of women in the labor market require post-breast cancer therapeutic adjustments. Hence, the aim of this study was to analyze HRQoL among Chilean breast cancer survivors, in general and considering geographic location of the participants (South, North, and North-Central Macroregions). In addition, to correlate HRQoL with age, education level and body mass index (BMI).
METHOD
Multicentric cross-sectional observational study approved by the Institutional Review Board of Servicio de Salud Metropolitano Oriente on August 8th, 2015. The STROBE cross-sectional checklist was adopted for this study.
Participants were recruited by trained health professionals (nurses, physiotherapists) who reviewed daily patient´s appointment registries and applied eligibility criteria. All the participants who voluntarily agreed to participate signed an Informed Consent Form. Four skilled physical therapists of the participant institutions collected the data and applied the questionnaires. Data collection was performed between 2015 and 2017.
The population of the study consists in female breast cancer survivors at three Chilean public Hospitals in three different Macroregions of the country: South (Complejo Asistencial Victor Rios Ruiz, Los Angeles), Central (Hospital del Salvador, Santiago de Chile), and North Central (Hospital de Quilpué, Quilpué). The reason why the three hospitals were selected was because they are located in the three most populous regions of the country. All eligible women were invited. The sample was composed with all the women who accepted to take part in the study. Exclusion criteria were women with cognitive deficit (abbreviated Chilean Version of the Mini-Mental State Examination scores lower than 13)14 preventing them to respond to the questionnaires, patients at palliative care for terminal cancer, and women whose clinical instability required hospitalization. Only two women were excluded because they were in palliative care for advanced cancer. All women that complied with eligibility criteria were invited and none refused to participate. The information contained in the clinical history was used to complement the information obtained from the patients.
The Chilean National Cancer Plan15 covers five Macroregions: North (Arica, Iquique, Antofagasta and Atacama), North Central (Coquimbo, Valparaíso - San Antonio, Viña del Mar – Quillota and Aconcagua), Central (Santiago Metropolitan south, north, central, orient and occident health services), South Central (O'Higgins and Maule), South (Ñuble, Concepción, Talcahuano, Biobío, Arauco and Araucanía Norte), and Extreme South (Araucanía Sur, Valdivia, Osorno, Del Reloncaví, Chiloé, Aysén y Magallanes)15. Santiago is Chile’s capital and the most populated area, hosting almost one third of the Chilean population and concentrating great part of the national production. Los Angeles is in the Biobío Region, the second most populated area, predominantly agricultural and home to indigenous population (mainly Mapuche). On its turn, Quilpué falls under the metropolitan area of Greater Valparaiso, which is the third most populated conurbation in the country whose main economic activities are industry, commerce, and services.
HRQoL was assessed using two questionnaires designed by the European Organization for Research and Treatment of Cancer (EORTC) group: The EORTC Quality of Life Questionnaire Core 30 (QLQ-C30) and the specific module for breast cancer (QLQ-BR23)16. Both were applied with a form during an interview using the validated Chilean versions17.
The EORTC QLQ-C30 is a general 30-items HRQoL questionnaire designed for cancer patients with the following domains: general health status, functioning (physical, role, emotional, cognitive and social), symptoms (fatigue, nausea, pain, dyspnea, insomnia, appetite loss, constipation, diarrhea, and financial burden). The scale ranges from 0 to 100, individual scores for functioning are worse when nearer to 0, while individual scores for symptoms are worse when nearer to 10016. The summary score is calculated according to the EORTC group guidelines18.
The EORTC QLQ-BR23 is a 23-itens instrument specific for breast cancer. The questionnaire addresses symptoms and functional scales. The score ranges from 0 to 100, wherein higher scores mean better results for functional scales and worse results for symptoms17.
Sociodemographic and clinical characteristics were obtained from patients’ hospital charts (age, income, country region, cancer stage, metastasis, chemotherapy, and radiotherapy) or were self-reported by patients (education level, occupation). Body mass index (BMI) was obtained through a physical evaluation of body mass (Kg) and body height (cm).
SPSS version 23 (IBM Corp., Armonk, NY, USA, 2011) with descriptive resources was used to analyze the data. For descriptive analysis frequencies, mean (standard deviation), and median (interquartile range) were used. To compare HRQoL between women from the three Macroregion hospitals, one-way ANOVA or Kruskall Wallis test was utilized wherein the case variables did not meet assumptions of normality or variance homogeneity. A radar chart was used to visualize the mean of the HRQoL summary score for the different regions. Missing values were not replaced as there were very few of them. All tests considered a significance threshold of p<0.05.
RESULTS
This study included 125 breast cancer survivors of different education levels and cancer stages at diagnosis, who attended physical therapy rehabilitation at three Chilean public hospitals (Table 1). All the eligible women accepted to participate upon invitation. The most frequent comorbidities were hypertension (n=47, 37.6%) and diabetes mellitus (n=30; 24%). All participants had undergone surgery (n=125, 100%), and most of them also received chemotherapy (n=89, 71.2%) and radiotherapy (n=65, 52%).
|
Table 1. Sociodemographic and disease-related characteristics of the study participants (n=125) |
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
Captions: Range A = Homeless or underprivileged individuals; Range B = Monthly taxable income less than or equal to CLP$ 250,000 (CLP = Chilean Pesos) and pensions; Range C = Monthly taxable income greater than CLP$ 250,000 and less than or equal to CLP$ 365,000; Range D = Monthly taxable income greater than CLP$ 365,001. (*) FONASA category = Fondo Nacional de Salud (Chilean National Public Insurance System); (#) This variable had 8 missing cases. |
The mean of the HRQoL summary score was 67.6 (SD=21.9; Md (Median)=71). Descriptive data of HRQoL from the total participants and from each of the regions is portrayed on Table 2. Concerning functioning domains, emotional functioning showed the lowest score (Md=58.3) while physical functioning had better scores (Md=80). Women´s appreciation of their general health was moderate (Md=50). Regarding symptoms, the most reported were pain (Md=50) and insomnia (Md=66.7), but fatigue, dyspnea, appetite loss, constipation, financial difficulties, breast and arm symptoms were also present (all of them with a median score of 33.3).
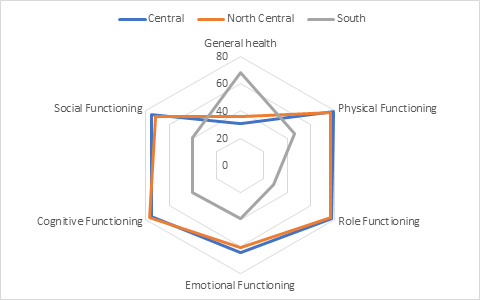
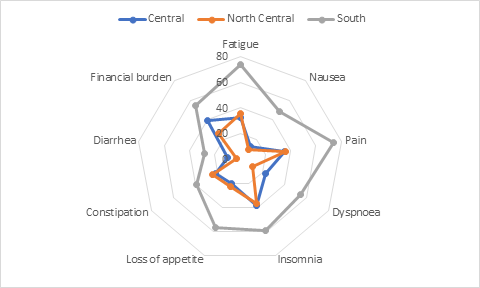
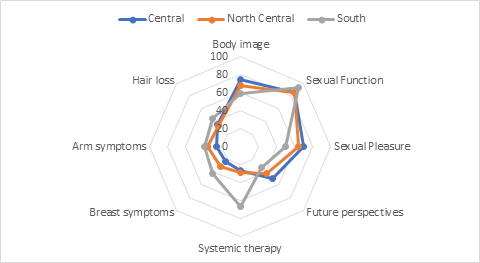
Women from the South Macroregion Hospital showed significantly lower scores for functioning domains and higher scores for symptoms compared with women from the North and Central-North Macroregions Hospitals (Figures 1, 2, and 3). In addition, women from the South Macroregion Hospital (Los Angeles, Biobio province) had significantly higher BMI and waist to hip ratio compared with those from the Central and North Central Macroregions Hospitals.
|
Table 2. Comparison of Quality-of-Life domains, age, and anthropometric indicators among women from three Chilean Macroregion Hospitals (n=125) |
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
Captions: MD = median; IR= interquartile range. |
|
|
|
Figure 1. Mean scores of functioning domains of health-related quality of life of breast cancer survivors from three different Chilean Macroregions. Higher scores mean better functioning (n=125) |
|
|
|
Figure 2. Mean scores of symptom domains of health-related quality of life of breast cancer survivors from three different Chilean Macroregions. Higher scores mean worse symptoms (n=125)
|
|
|
|
Figure 3. Mean scores of breast cancer specific domains of health-related quality of life of breast cancer survivors from three different Chilean Macroregions. Left: Higher scores mean better function. Right: Higher scores mean worse symptoms (n=125)
|
The summary mean score of HRQoL was significantly correlated to age (Spearman´s rho=.202, p=.033), BMI (Spearman´s rho=-.341, p<.001), and education level (Spearman´s rho=.310, p=.001).
DISCUSSION
This study shows that HRQoL of Chilean Breast Cancer survivors declined mainly in emotional functioning, the domain with the lowest score similar to other studies19,20. Educational interventions may contribute to solve this situation, improving patients’ sense of mastery, and enhancing their emotional well-being and overall sense of HRQoL8. In addition, effective health promotion contributes to early detection, and to improve survival and HRQoL. Favorable strategies include compliance to cancer screening guidelines, early detection and treatment, and prevention (physical activity, body weight control, and healthy diet)21.
Pain and insomnia were the most reported symptoms. Fatigue, dyspnea, appetite loss, constipation, financial difficulties, breast and arm symptoms were also present. In line with the results, an overview of systematic reviews described that the most frequently reported bothersome symptoms in breast cancer survivors were fatigue, insomnia, depression, cognitive dysfunction, reproductive and menopausal symptoms, and lymphedema22. According to a recently published review23, insomnia is highly prevalent among patients with breast cancer, being influenced by endocrine therapy and hot flashes, pain and discomfort from local therapy, and fear of recurrence.
Reducing the burden of these symptoms should be a priority for health care systems. Currently, there is evidence that physical exercise is strongly recommended to manage cancer related fatigue24 and cognitive behavioral therapy has been shown to be useful in reducing insomnia and improving sleep quality in women treated for breast cancer25. In addition, physical activity, lymphedema management and psychosocial interventions demonstrated to be effective in improving quality of life22. However, the actual challenge is to make these interventions available to breast cancer survivors.
HRQoL was negatively correlated to BMI. In Chile, excess body weight is a common health problem, as 34.4% of the population are obese and 39.8% are overweight26. According to a recent study9 that included only obese women receiving treatment for early-stage breast cancer, those who lost weight experienced a lesser decline in this index, reporting better physical function, less dyspnea, less pain, and fewer breast symptoms when compared with gaining weight or remaining stable.
The higher the education level and age the better women´s QoL. Education level is an indicator of socioeconomic status. Accordingly, a large epidemiological cohort study from Barcelona/Spain7 concluded that QoL of breast cancer survivors is closely related to their socioeconomic status, where the poorest results are from the women of the most disadvantaged classes and those in social isolation.
Women from the South Macroregion Hospital had lower HRQoL, income and education levels compared with those from the Central and Central North Macroregions. Although this study does not have a representative sample, results might indicate that regional differences concerning the QoL exist, also representing health inequalities. The Chilean observatory of public health created an index of socioeconomic development to classify the cities (“comunas”) of the country, including the following indicators: economy (per capita income and poverty rate), educational level, life expectancy, Human Development Index, years of life lost, Swaroop index (rate used to compare mortality between populations with different age structures) and child mortality rate27. By using this classification, it is possible to conclude that the cities from the South Macroregion Hospital (Los Angeles) showed the lowest values varying from 0.280 (the worst country score) to 0.580. Meanwhile the cities of the Central North Macroregion (Hospital de Quilpué) had high to moderate values, ranging from 0.668 to 0.712; and the Central Macroregion (Hospital del Salvador) showed the higher values, ranging from 0.668 to 0.992, the sixth of the first seven better positions of the country.
Addressing socio-economical aspects and improving equality in the health care access, including screening and timely treatment, is fundamental in reducing the worldwide burden of breast cancer2. It has been suggested that interventions with social support and social constraints play an important role mediating the relationship between socioeconomic inequalities and HRQoL28. Survivorship care plans should take into consideration regional diversity among breast cancer survivors. Currently, such approaches can be more easily implemented as telemedicine or telerehabilitation is advancing and providing support for individuals needing cancer rehabilitation care29.
This study has some limitations, such as lack of information regarding patients´ time since their breast cancer diagnosis and age at diagnosis, and inclusion of public health system patients only. Additionally, the small sample size impeded further analyzes of subgroups and does not mirror the total population. As a strength, it contributes to oncology by showing that HRQoL of Chilean breast cancer survivors has impairments. This knowledge is relevant for developing supportive care plans for breast cancer survivors. For future studies it is suggested population-based studies addressing control of socioeconomic, cultural and demographic factors.
CONCLUSION
This multicentric study showed that Chilean breast cancer survivors had some impairment in their HRQoL, mainly regarding emotional functioning and symptoms (pain, insomnia, fatigue, dyspnea, appetite loss, constipation, financial difficulties, breast and arm symptoms). There were regional differences in HRQoL. The summary mean score of HRQoL correlated positively to age and education level but correlated negatively to BMI. This scenario suggests that continuous activities for breast cancer survivors may facilitate early comprehensive rehabilitation and reinsertion in the society. In this context, the role of health education of women targeting self-care strategies would avoid the precariousness of their clinical health, in the short and long term.
CONTRIBUTIONS
Luz Alejandra Lorca, Sandra Vera-Llanos and Alicia Estefanía Hinrichsen-Ramírez designed the study. Luz Alejandra Lorca, Sandra Vera-Llanos, Alicia Estefanía Hinrichsen-Ramírez, Karen López, Marcela Veja and Patricia Contalba recollected data. Cinara Sacomori, Luz Alejandra Lorca and Fabiana Flores Sperandio analyzed data and wrote the manuscript. All the authors revised and approved the final manuscript.
DECLARATION OF CONFLICT OF INTERESTS
There is no conflict of interests to declare.
None.
REFERENCES
1. Bray F, Ferlay J, Soerjomataram I, et al. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68(6):394-424. doi: https://doi.org/10.3322/caac.21492
2. Tao ZQ, Shi A, Lu C, et al. Breast cancer: epidemiology and etiology. Cell Biochem Biophys. 2015;72(2):333-8. doi: https://doi.org/10.1007/s12013-014-0459-6
3. Ministerio de Salud (CL), Subsecretaría de Salud Pública, División de prevención y Control de Enfermedades, Departamento Manejo Integral del Cáncer y otros Tumores. Guías clínicas AUGE: cáncer de mama. Santiago (CL): Minsal; 2015.
4. Miller AM, Ashing KT, Modeste NN, et al. Contextual factors influencing health-related quality of life in African American and Latina breast cancer survivors. J Cancer Surviv. 2015;9(3):441-9. doi: https://doi.org/10.1007/s11764-014-0420-0
5. Sibhat SG, Fenta TG, Sander B, et al. Health-related quality of life and its predictors among patients with breast cancer at Tikur Anbessa Specialized Hospital, Addis Ababa, Ethiopia. Health Qual Life Outcomes. 2019;17(1):165. doi: https://doi.org/10.1186/s12955-019-1239-1
6. Sitlinger A, Zafar SY. Health-related quality of life: the impact on morbidity and mortality. Surg Oncol Clin N Am. 2018;27(4):675-84. doi: https://doi.org/10.1016/j.soc.2018.05.008
7. Graells-Sans A, Serral G, Puigpinós-Riera R. Social inequalities in quality of life in a cohort of women diagnosed with breast cancer in Barcelona (DAMA Cohort). Cancer Epidemiol. 2018;54:38-47. doi: https://doi.org/10.1016/j.canep.2018.03.007
8. Fischer MJ, Inoue K, Matsuda A, et al. Cross-cultural comparison of breast cancer patients’ quality of life in the Netherlands and Japan. Breast Cancer Res Treat. 2017;166(2):459-71. doi: https://doi.org/10.1007/s10549-017-4417-z
9. Di Meglio A, Michiels S, Jones LW, et al. Changes in weight, physical and psychosocial patient-reported outcomes among obese women receiving treatment for early-stage breast cancer: a nationwide clinical study. Breast. 2020;52:23-32. doi: https://doi.org/10.1016/j.breast.2020.04.002
10. Wang L, Guyatt GH, Kennedy SA, et al. Predictors of persistent pain after breast cancer surgery: a systematic review and meta-analysis of observational studies. CMAJ. 2016;188(14):E352-E61. doi: https://doi.org/10.1503/cmaj.151276
11. Nguyen-Pham S, Leung J, McLaughlin D. Disparities in breast cancer stage at diagnosis in urban and rural adult women: a systematic review and meta-analysis. Ann Epidemiol. 2014;24(3):228-35. doi: https://doi.org/10.1016/j.annepidem.2013.12.002
12. Andrade MC, Ribeiro AP, Lanza K, et al. Ações de detecção precoce do câncer de mama no brasil: análise dos dados do sistema de informação do controle do câncer de mama (Sismama), 2009-2015. Rev Bras Cancerol. 2022;68(3):e-082189. doi: https://doi.org/10.32635/2176-9745.rbc.2022v68n3.2189
13. Gonzalez L, Bardach A, Palacios A, et al. Health-related quality of life in patients with breast cancer in latin america and the caribbean: a systematic review and meta-analysis. Oncologist. 2021;26(5):e794-e806. doi: https://doi.org/10.1002/onco.13709
14. Jiménez D, Lavados M, Rojas P, et al. Evaluación del minimental abreviado de la evaluación funcional del adulto mayor (EFAM) como screening para la detección de demencia en la atención primaria. Rev Med Chil. 2017;145(7):862-8. doi: http://doi.org/10.4067/s0034-98872017000700862
15. Ministerio de Salud (CL). Plan Nacional de Cáncer 2018-2028 [Internet]. Santiago (CL): Ministerio de Salud; 2018 [acesso 2022 mar 10]. Disponível em: https://www.minsal.cl/wp-content/uploads/2019/01/2019.01.23_PLAN-NACIONAL-DE-CANCER_web.pdf
16. Aaronson NK, Ahmedzai S, Bergman B, et al. The European Organization for research and treatment of cancer QLQ-C30: a quality-of-life instrument for use in international clinical trials in oncology. J Natl Cancer Inst. 1993;85(5):365-76. doi: https://doi.org/10.1093/jnci/85.5.365
17. Irarrázaval ME, Rodríguez PF, Fasce G, et al. Calidad de vida en cancer de mama: validacion del cuestionario BR23 en Chile. Rev Med Chil. 2013;141(6):723-34. doi: https://doi.org/10.4067/S0034-98872013000600006
18. Husson O, de Rooij BH, Kieffer J, et al. The EORTC QLQ-C30 summary score as prognostic factor for survival of patients with cancer in the “Real-World”: results from the population-based PROFILES registry. Oncologist. 2020;25(4):e722-e32. doi: https://doi.org/10.1634/theoncologist.2019-0348
19. Imran M, Al-Wassia R, Alkhayyat SS, et al. Assessment of quality of life (QoL) in breast cancer patients by using EORTC QLQ-C30 and BR-23 questionnaires: a tertiary care center survey in the western region of Saudi Arabia. PLoS One. 2019;14(7):e0219093. doi: https://doi.org/10.1371/journal.pone.0219093
20. El Fakir S, El Rhazi K, Zidouh A, et al. Health-related quality of life among breast cancer patients and influencing factors in Morocco. Asian Pac J Cancer Prev. 2016;17(12):5063-9. doi: https://doi.org/10.22034/APJCP.2016.17.12.5063
21. Agide FD, Sadeghi R, Garmaroudi G, et al. A systematic review of health promotion interventions to increase breast cancer screening uptake: from the last 12 years. Eur J Public Health. 2018;28(6):1149-1155. doi: https://doi.org/10.1093/eurpub/ckx231
22. Mokhtari-Hessari P, Montazeri A. Health-related quality of life in breast cancer patients: review of reviews from 2008 to 2018. Health Qual Life Outcomes. 2020;18(1):338. doi: https://doi.org/10.1186/s12955-020-01591-x
23. Kwak A, Jacobs J, Haggett D, et al. Evaluation and management of insomnia in women with breast cancer. Breast Cancer Res Treat. 2020;181(2):269-77. doi: https://doi.org/10.1007/s10549-020-05635-0
24. Jiang M, Ma Y, Yun B, et al. Exercise for fatigue in breast cancer patients: an umbrella review of systematic reviews. Int J Nurs Sci. 2020;7(2):248-54. doi: https://doi.org/10.1016/j.ijnss.2020.03.001
25. Ma Y, Hall DL, Ngo LH, et al. Efficacy of cognitive behavioral therapy for insomnia in breast cancer: a meta-analysis. Sleep Med Rev. 2021;55:101376. doi: https://doi.org/10.1016/j.smrv.2020.101376
26. Ministerio de Salud (CL), Departamento de Epidemiología, División de Planificación Sanitaria, Subsecretaría de Salud Pública. Encuesta Nacional de Salud 2016-2017 [Internet]. Santiago (CL): Ministerio de Salud; 2017 [acesso 2022 mar 10]. Disponível em: https://www.minsal.cl/wp-content/uploads/2017/11/ENS-2016-17_PRIMEROS-RESULTADOS.pdf
27. Observatorio Chileno de Salud Publica [Internet]. Santiago (CL): OCHISAP; [data desconhecida]. Nivel socioeconómico y de salud de las comunas de Chile; [2013]. [acesso 2022 mar 10]. Disponível em: http://www.ochisap.cl/index.php/nivel-socioeconomico-y-de-salud-de-las-comunas-de-chile
28. You J, Wang C, Yeung NCY, et al. Socioeconomic status and quality of life among Chinese American breast cancer survivors: the mediating roles of social support and social constraints. Psychooncology. 2018;27(7):1742-9. doi: https://doi.org/10.1002/pon.4719
29. Galiano-Castillo N, Cantarero-Villanueva I, Fernández-Lao C, et al. Telehealth system: a randomized controlled trial evaluating the impact of an internet-based exercise intervention on quality of life, pain, muscle strength, and fatigue in breast cancer survivors. Cancer. 2016;122(20):3166-74. doi: https://doi.org/10.1002/cncr.30172
Recebido em 27/6/2022
Aprovado em 3/10/2022
Scientific-Editor: Anke Bergmann. Orcid iD: https://orcid.org/0000-0002-1972-8777
![]()
Este é um artigo publicado em acesso aberto (Open Access) sob a licença Creative Commons Attribution, que permite uso, distribuição e reprodução em qualquer meio, sem restrições, desde que o trabalho original seja corretamente citado.
©2019 Revista Brasileira de Cancerologia | Instituto Nacional de Câncer | Ministério da Saúde