CASE REPORT
Challenging Diagnosis of Low-grade Fibromyxoid Sarcoma of the Chest Wall: Case Report
Diagnóstico Desafiador de Sarcoma Fibromixoide de Baixo Grau de Parede Torácica: Relato de Caso
Diagnóstico Desafiante de Sarcoma Fibromixoide de Bajo Grado de Pared Torácica: Informe de Caso
doi: https://doi.org/10.32635/2176-9745.RBC.2023v69n2.3288
Rafael Everton Assunção Ribeiro da Costa1; Ana Carolina Vieira Mendes2; Eugênio de Sá Coutinho Neto3; Raimundo Gerônimo da Silva Júnior4; Cromwell Barbosa de Carvalho Melo5; José Santana Moreira Ramos Júnior6; Sabas Carlos Vieira7; Carlos Eduardo Coelho de Sá8
1Universidade Estadual do Piauí, Centro de Ciências da Saúde. Teresina (PI), Brazil. E-mail:rafaelearcosta@gmail.com. Orcid iD:https://orcid.org/0000-0002-0798-890X
2Universidade Estadual do Maranhão, Centro de Ciências da Saúde. Caxias (MA), Brazil. E-mail:anacarolinavieiramendes@gmail.com. Orcid iD:https://orcid.org/0000-0003-3761-4543
3,5,6Hospital Macrorregional de Caxias Dr. Everardo Aragão, Unidade de Alta Complexidade em Oncologia. Caxias (MA), Brazil. E-mails: eugeniocoutinhoneto@gmail.com; cromwellmelo@hotmail.com; nctorax@gmail.com. Orcid iD: https://orcid.org/0000-0002-0806-3933; Orcid iD: https://orcid.org/0000-0002-0148-9413; Orcid iD: https://orcid.org/0000-0003-1170-4719
4Universidade Federal do Piauí, Centro de Ciências da Saúde. Teresina (PI), Brazil. E-mail: gerjrpi@gmail.com. Orcid iD: https://orcid.org/0000-0003-4032-6710
7Oncocenter. Teresina (PI), Brazil. E-mail: drsabasvieira@gmail.com. Orcid iD: https://orcid.org/0000-0003-0935-7316
8Hospital Macrorregional de Caxias Dr. Everardo Aragão, Unidade de Alta Complexidade em Oncologia. Caxias (MA), Brazil. Oncocenter. Teresina (PI), Brazil. E-mail: eduardo_sa1601@hotmail.com. Orcid iD: https://orcid.org/0000-0002-9610-8010
Corresponding author: Rafael Everton Assunção Ribeiro da Costa. Rua Olavo Bilac, 2335 – Centro (Sul). Teresina (PI), Brazil. E-mail: rafaelearcosta@gmail.com
ABSTRACT
Introduction: Low-grade fibromyxoid sarcoma (LGFMS) is a rare special subtype of fibrosarcoma, it is more common in the trunk and proximal limbs. First described by Evans in 1987, this tumor is also named Evans tumor. Diagnosis of LGFMS may be quite challenging, either due to the low suspicion rate of the tumor or low specificity of its morphological pattern and immunohistochemical profile, a phenomenon that is magnified when tumor location is less usual, such as in the chest wall. The present article presents a challenging case of LGFMS of the chest wall. Case report: Female, 58-year-old patient was referred to the oncology referral clinic with a breast tumor. Diagnostic investigation included imaging tests (breast US and chest CT scan) and core needle biopsy. CT scan revealed the epicenter of the tumor in the left anterior thoracic wall. Biopsy to evaluate the histologic type of tumor was carried out and the result was inconclusive. Therefore, surgical excision of the tumor was performed. Histopathology and immunohistochemistry studies of the surgical specimen confirmed the diagnosis of LGFMS of the chest wall. Currently, after 36 months of the surgical excision, the patient is still doing well and continues under clinical follow-up. Conclusion: Although the diagnosis of LGFMS of the chest wall is challenging, it should be done correctly, since these cases require a long and thorough clinical follow-up.
Key words: sarcoma; thoracic wall; immunohistochemistry; diagnosis, differential; case reports.
RESUMO
Introdução: O sarcoma fibromixoide de baixo grau (SFBG) é um subtipo especial de fibrossarcoma de ocorrência rara, sendo mais frequente em tronco e parte proximal dos membros. Esse tumor, primeiramente descrito por Evans em 1987, também pode ser chamado de “tumor de Evans”. O diagnóstico de SFBG pode ser bastante desafiador tanto por ser um tumor pouco suspeitado como pelo fato de seu padrão morfológico e perfil imuno-histoquímico serem pouco específicos, fenômeno magnificado quando a localização é menos usual, como na parede torácica. O presente artigo apresenta um caso desafiador de SFBG de parede torácica. Relato do caso: Paciente, sexo feminino, 58 anos, foi encaminhada ao serviço de referência em oncologia com tumor em região mamária. Realizou-se investigação diagnóstica com exames de imagens (ultrassonografia das mamas e tomografia computadorizada – TC de tórax) e biópsia por agulha grossa. A TC de tórax evidenciou que o tumor tinha epicentro na parede torácica anterior esquerda. Não houve conclusão sobre o tipo histológico do tumor. Foi realizada excisão cirúrgica. O histopatológico e a imuno-histoquímica da peça cirúrgica permitiram o diagnóstico de SFBG de parede torácica. Atualmente, 36 meses após a excisão do tumor, a paciente está bem e em seguimento clínico. Conclusão: Apesar de o diagnóstico de um SFBG de parede torácica ser desafiador, é importante realizá-lo adequadamente, uma vez que esses casos exigem um seguimento clínico longo e minucioso.
Palavras-chave: sarcoma; parede torácica; imuno-histoquímica; diagnóstico diferencial; relatos de casos.
RESUMEN
Introducción: El sarcoma fibromixoide de bajo grado (SFBG) es un subtipo especial de fibrosarcoma de rara aparición, siendo más frecuente en tronco y parte proximal de las extremidades. Descrito por primera vez por Evans en 1987, este tumor también ha sido llamado tumor de Evans. El diagnóstico de un SFBG puede ser bastante desafiante, tanto porque es un tumor poco sospechado como porque su patrón morfológico y perfil inmunohistoquímico son poco específicos, fenómeno magnificado cuando la localización del tumor es inusual, como en la pared torácica. El objetivo de este estudio es informar un caso desafiante de SFBG de pared torácica. Informe del caso: Una paciente de 58 años con un tumor en la mama fue derivada al centro de referencia de oncología. La investigación diagnóstica incluyó pruebas de imagen (US de mama y TC de tórax) y biopsia con aguja gruesa. La TC de tórax reveló el epicentro del tumor en la pared torácica anterior izquierda. Se realizó biopsia del tipo histológico de tumor el y el resultado no fue concluyente. Por lo tanto, se realizó la extirpación quirúrgica del tumor. Los estudios de histopatología e inmunohistoquímica de la pieza quirúrgica confirmaron el diagnóstico de SFBG de pared torácica. Actualmente, a los 36 meses de la extirpación quirúrgica, la paciente sigue evolucionando bien y continúa en seguimiento clínico. Conclusión: Aunque el diagnóstico de un SFBG de pared torácica es desafiante, es importante realizarlo adecuadamente, ya que estos casos requieren un seguimiento clínico prolongado y exhaustivo.
Palabras clave: sarcoma; pared torácica; inmunohistoquímica; diagnóstico diferencial; informes de casos.
INTRODUCTION
Fibrosarcoma is a type of soft tissue sarcoma that is more common in middle-aged and older adults, rarely occurring in children. Typically, the tumor most affects soft tissues of the limbs, trunk, head and neck. In the last decades, this pathology has evolved, and it was possible to conclude that fibrosarcomas represent only about 3.6% of soft tissue sarcomas in adults, worldwide. The remaining sarcomas consists of other tumor variants, such as: 1) low-grade fibromyxoid sarcoma (LGFMS); 2) sclerosing epithelioid fibrosarcoma; 3) dermatofibrosarcoma protuberans; 4) dermatofibrosarcoma fibrosarcomatous protuberans; 5) monophasic synovial sarcoma; 6) other neoplasms of fusiform cells that may mimic fibrosarcoma1.
Therefore, LGFMS represents a rare and special subtype of fibrosarcoma. Initially described by Evans in 1987, this tumor was also known as Evans tumors. However, since 1993 the official nomenclature of these tumors is LGFMS2,3.
As described by Evans and others, the morphological diagnosis of a LGFMS may be challenging, due to its typically low cellularity, abundant collagen and relatively bland cytology. In most cases, a circumscribed and subtly infiltrative growth pattern is observed. The tumor consists of a mixture of heavily collagenized hypocellular zones and myxoid nodules, showing a higher cellularity, spiral growth pattern and curvilinear vessels. The “abrupt” transition from collagenized zones to myxoid nodules and presence of small vessels the size of arterioles with concentric hyalinization and distorted lumen are important clues for diagnosis.
Typically, LGFMS cells are relatively uniform and bland, although hyperchromatism and nuclear irregularity can become apparent on closer inspection. Mitotic activity is typically very low and necrosis is absent. In a very small number of cases, increased cellularity and nuclear atypia, hyalinization and alteration identical to that observed in sclerosing epithelioid fibrosarcoma, along with giant collagen rosettes may occur. On immunohistochemistry (IHC), LGFMS usually expresses vimentin. Epithelial membrane antigen (EMA) and MUC4 (a highly sensitive and relatively specific marker for LGFMS) expression may also occur, in addition to other markers1.
LGFMS occurs most frequently in the proximal limbs and trunk. Diagnosis of the tumor is challenging, since it has diverse morphologic patterns and a nonspecific immunohistochemical profile. Treatment of choice is surgical excision of the tumor with wide surgical margins. Chemotherapy and radiotherapy are not expected to have a significant effect on the long-term prognosis of these patients, due to the low mitotic index of LGFMS4.
The aim of this study is to report a case of low-grade fibromyxoid sarcoma of the chest wall which posed a challenging diagnosis.
CASE REPORT
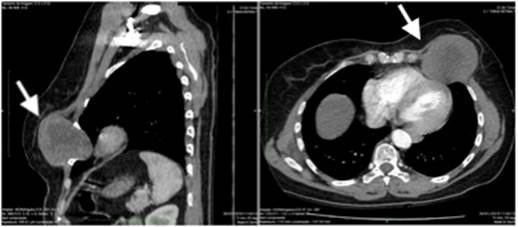
A 58-year-old woman was admitted to the oncology clinic of “Hospital Macrorregional Dr. Everaldo Ferreira Aragão” on 12/18/2018 due to the presence of a nearly 7-cm left breast tumor. The patient had no prior history of cancer and was taking medication for arterial hypertension. A breast ultrasonography (US) was performed after admission, showing a large mass in the left breast, measuring 6.5 cm (BI-RADS 4). A computed tomography (CT) scan of the chest was then indicated and performed on 1/30/2019, revealing an expansive growth with post-contrast enhancement and epicenter in the left anterior chest wall (Figure 1).
|
|
|
Figure 1. Chest computed tomography (CT) scan of the patient. Note: Arrows show a prominent soft tissue tumor of the chest wall |
A core needle biopsy (CNB) and hematoxylin-eosin (H&E) histopathology study were performed on 2/26/2019. Results showed a spindle cell lesion without atypia. The pathologist indicated IHC to test smooth muscle actin, CD34, AE1/AE3, desmin, S100 protein, p63, cytokeratin 8/18 and vimentin, which occurred on 4/16/2019. Tumor cells were positive only for vimentin protein. IHC showed a low-grade spindle cell tumor and a definitive diagnosis could not be made due to insufficient amount of tissue.
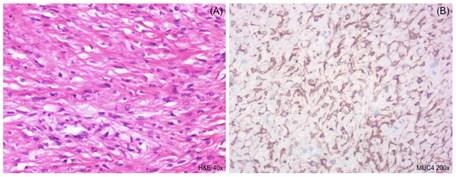
On 8/27/2019, the patient underwent tumor excision surgery. Tumor and bone tissue samples of 10 cm, along with a tumor lesion (7.3 cm in size) adherent to bone structure were submitted to the pathology laboratory. H&E histopathology analysis (Figure 2A) showed alternating patterns with hyper- and hypocellular areas, vascular proliferation with hyalinization in vascular walls, mitotic index of 2 mitoses/high-power field and no necrosis. Angiolymphatic and perineural invasion were not detected. Surgical margins were negative. IHC investigation was positive for EMA and MUC4 (Figure 2B). The pathologist reached the diagnosis of low-grade fibromyxoid sarcoma of the chest wall.
|
|
|
Figure 2. Histopathology and immunohistochemical analysis. (A): Hematoxylin-eosin (H&E) histopathology staining visualized in magnification of 40x. (B): Staining of MUC4 protein in magnification of 200x |
The patient was scheduled for periodical clinical follow-up care. At approximately 36 months after the tumor excision, she is currently doing well and has no evidence of malignancy or signs of relapse.
This Institutional Review Board of the “Universidade Estadual do Piauí”, Teresina (PI), Brazil – reference number 5.350.088 (CAAE: 57458922.8.0000.5209) approved the study. The patient signed the informed consent form (ICF).
DISCUSSION
LGFMS of the chest wall is a very rare tumor and few cases have been reported in the world literature. Clinical presentation can vary according to the exact tumor location. However, LGFMS is commonly a slow-growing, asymptomatic tumor frequently diagnosed by imaging tests5.
Furthermore, LGFMSs are usually well-delimited tumors, measuring 1 to 23 cm (median, 9.5 cm). Histopathology study of these tumors shows that spindle cells resemble fibroblasts, heavily collagenized hypocellular zones and richly cellular myxoid nodules. Short or typically whorled growth patterns, blood vessel proliferation accompanied by perivascular hyaline degeneration and necrosis may also be observed. IHC should be performed in these cases. On IHC, the most specific markers for LGFMS to date are vimentin, CD99, Bcl-2 and MUC4, as occurred in the current case, where tumor cells were positive for MUC4 and vimentin expression. On the other hand, EMA, keratin, desmin, SMA, S100, CD34 and myogenin usually have negative results. The main differential diagnoses of LGFMS in histopathology studies are: sclerosing epithelioid fibrosarcoma, solitary fibrous tumor, low-grade myxofibrosarcoma, myofibroblastoma of the breast, malignant or borderline phyllodes tumor and myxoid liposarcoma4.
LGFMSs are aggressive tumors with recurrence, metastasis and death rates of 64%, 45% and 42%, respectively6. Nevertheless, treatment options for these tumors remain limited. Some individuals do not respond to the currently available chemotherapy and radiotherapy regimens. Surgical resection and long-term periodical clinical follow-up are still the only treatment modalities available6,7.
This study is relevant because it reports a case with a very challenging diagnosis. At the time of the diagnostic hypothesis, LGFMS may not come to mind when a chest mass is detected on imaging tests. Furthermore, morphological and immunohistochemical data may not be very specific, particularly in biopsy samples. In this case, H&E histopathology study and IHC in the CNB sample failed to reach the diagnosis of LGFMS. Although adjuvant therapy is limited in these cases, it is fundamental to investigate the definitive diagnosis using material obtained by wide surgical tumor excision. LGFMSs are associated with a high recurrence/metastasis rate. As a result, periodical long-term clinical follow-up is recommended in these patients.
CONCLUSION
The diagnosis of low-grade fibromyxoid sarcoma of the chest wall can be challenging. Nevertheless, it is important to continue diagnostic investigation, since these patients will require a long and thorough clinical follow-up.
ACKNOWLEDGMENTS
To Hospital Macrorregional Dr. Everaldo Ferreira Aragão, Caxias (MA) for institutional support.
CONTRIBUTIONS
Rafael Everton Assunção Ribeiro da Costa, Ana Carolina Vieira Mendes contributed to the study design, data acquisition, quality control, data analysis and interpretation, wording and review. Eugênio de Sá Coutinho Neto, Raimundo Gerônimo da Silva Júnior, Cromwell Barbosa de Carvalho Melo, José Santana Moreira Ramos Júnior, Sabas Carlos Vieira, Carlos Eduardo Coelho de Sá contributed to the study design, acquisition, quality control, analysis and interpretation of the data, wording, and critical review. All the authors approved the final version to be published.
DECLARATION OF CONFLICT OF INTERESTS
There is no conflict of interest to declare.
FUNDING SOURCES
None.
REFERENCES
1. Folpe AL. Fibrosarcoma: a review and update. Histopathology. 2014;64(1):12-25. doi: https://doi.org/10.1111/his.12282
2. Evans HL. Low-grade fibromyxoid sarcoma. A report of two metastasizing neoplasms having a deceptively benign appearance. Am J Clin Pathol. 1987;88(5):615-9. doi: https://doi.org/10.1093/ajcp/88.5.615
3. Evans HL. Low-grade fibromyxoid sarcoma. A report of 12 cases. Am J Surg Pathol. 1993;17(6):595-600. doi: https://doi.org/10.1097/00000478-199306000-00007
4. Zhang Y, Wan D, Gao F. Primary low-grade fibromyxoid sarcoma of the breast: a rare case report with immunohistochemical and fluorescence in situ hybridization detection. Hum Pathol. 2018;79:208-11. doi: https://doi.org/10.1016/j.humpath.2018.02.013
5. Perez D, El-Zammar O, Cobanov B, et al. Low-grade fibromyxoid sarcoma: a rare case in an unusual location. SAGE Open Med Case Rep. 2020;8:2050313X20944315. doi: https://doi.org/10.1177/2050313X20944315
6. Park JM, Lim HR, Kim JH, et al. Giant low-grade fibromyxoid sarcoma in the neck. Korean J Otorhinolaryngol-Head Neck Surg. 2020;63(9):432-5. doi: https://doi.org/10.3342/kjorl-hns.2019.00857
7. Chamberlain F, Engelmann B, Al-Muderis O, et al. Low-grade fibromyxoid sarcoma: treatment outcomes and efficacy of chemotherapy. In Vivo. 2020;34(1):239-45. doi: https://doi.org/10.21873/invivo.11766
Recebido em 12/9/2022
Aprovado em 7/2/2023
Associate-Editor: Claudio Gustavo Stefanoff. Orcid iD: https://orcid.org/0000-0001-7050-3269
Scientific-Editor: Anke Bergmann. Orcid iD: https://orcid.org/0000-0002-1972-8777
![]()
Este é um artigo publicado em acesso aberto (Open Access) sob a licença Creative Commons Attribution, que permite uso, distribuição e reprodução em qualquer meio, sem restrições, desde que o trabalho original seja corretamente citado.
©2019 Revista Brasileira de Cancerologia | Instituto Nacional de Câncer | Ministério da Saúde