CASE REPORT
Radiation-Induced Undifferentiated Pleomorphic Sarcoma after Breast Conserving Therapy: Case Report
Sarcoma Pleomórfico de Mama Radioinduzido Pós-Tratamento Conservador de Câncer de Mama Inicial: Relato de Caso
Sarcoma Pleomórfico de Mama Radioinducido tras Tratamiento Conservador de Cáncer de Mama Inicial: Informe de Caso
doi: https://doi.org/10.32635/2176-9745.RBC.2023v69n2.3557
Tainara Rodrigues Miranda1; Marie Nathalie Chenu2; Camila de Carvalho Figueiredo3; Marcelo Morais Barbosa4; Patricia Chaves de Freitas Campos Jucá5
1-5Instituto Nacional de Câncer (INCA), Hospital do Câncer III (HC III). Rio de Janeiro (RJ), Brazil.
1E-mail: tainara_miranda@hotmail.com. Orcid iD: https://orcid.org/0000-0001-5278-6883
2E-mail: mnchenu@gmail.com. Orcid iD: https://orcid.org/0000-0002-8898-6585
3E-mail: camilac.figueiredo@gmail.com. Orcid iD: https://orcid.org/0000-0002-6267-9376
4E-mail: marcelomoraisb@yahoo.com.br. Orcid iD: https://orcid.org/0000-0001-8654-8269
5E-mail: patriciacjuca@gmail.com. Orcid iD: https://orcid.org/0000-0003-3190-6326
Corresponding author: Tainara Rodrigues Miranda. Rua Visconde de Pirajá, 300, apto. 801 – Ipanema. Rio de Janeiro (RJ), Brazil. CEP 22410-000. E-mail: tainara_miranda@hotmail.com
ABSTRACT
Introduction: Breast sarcoma is a rare form of malignancy that arises from connective tissue, comprising less than 5% of all sarcomas. Undifferentiated pleomorphic sarcoma (UPS) of the breast is a rare and aggressive subtype of radiation-induced sarcoma that can occur in treated breast cancer patients. The diagnosis is challenging and often missed due to the low incidence, long latency period, unspecific imaging finding, and difficulties in clinical and histological detection. Case report: A 56-year-old woman was diagnosed with early-stage triple-negative breast cancer in 2013 and underwent breast-conserving therapy (BCT). After five years follow-up, she developed mastalgia and breast induration, and after mammography and ultrasound without suspicious lesions, a magnetic resonance imaging (MRI) was performed and showed a highly suggestive malignancy mass measuring 8.0 cm and invading the chest wall. The core biopsy revealed a spindle cells malignant tumor, negative for pan cytokeratin and most of immuno-histochemical markers, suggesting sarcoma, but requiring investigation of surgical specimen to exclude metaplastic carcinoma. She underwent Halsted radical mastectomy, full-thickness left anterior chest wall resection contemplating segments of the 4th and 5th ribs and reconstruction with synthetic mesh. The surgical specimen evidenced a UPS with clear margins. The patient had good postoperative recovery and remains in follow-up with the mastology team. Conclusion: This report shows that radiation-induced sarcomas of the breast can be difficult to diagnose, and how later treatment can demand a major surgery with higher morbidity. Prognosis may improve if detected early.
Key words: sarcoma; breast neoplasms; neoplasms, radiation-induced; neoplasms, second primary; case reports.
RESUMO
Introdução: O sarcoma de mama é uma forma rara de câncer que surge do tecido conjuntivo, compreendendo menos de 5% de todos os sarcomas. O sarcoma pleomórfico indiferenciado (SPI) da mama é um subtipo raro e agressivo de sarcoma induzido por radiação que pode surgir em pacientes pós-tratamento conservador de câncer de mama. O diagnóstico é desafiador e, muitas vezes, tardio, em virtude da baixa incidência, longo período de latência, achados de imagem inespecíficos e dificuldades na detecção clínica e histológica. Relato do caso: Paciente do sexo feminino, 56 anos, foi diagnosticada com câncer de mama triplo-negativo estadiamento inicial em 2013 e submetida a tratamento conservador de câncer de mama. Após cinco anos de seguimento, evoluiu com mastalgia e endurecimento mamário e, após mamografia e ultrassonografia sem lesões suspeitas, foi realizada ressonância magnética que evidenciou massa altamente sugestiva de malignidade medindo 8,0 cm com invasão da parede torácica. O resultado da core biopsy revelou um tumor maligno de células fusiformes, negativo para pancitoqueratina e para a maioria dos marcadores imuno-histoquímicos, sugerindo sarcoma, mas exigindo estudo de peça cirúrgica para excluir carcinoma metaplásico. A paciente foi submetida à mastectomia radical de Halsted, ressecção da parede torácica anterior esquerda contemplando segmentos das 4ª e 5ª costelas e reconstrução com tela sintética. O laudo histopatológico da peça cirúrgica evidenciou SPI com margens livres. Evoluiu com boa recuperação pós-operatória, permanecendo em acompanhamento com a equipe de mastologia. Conclusão: O relato de caso ilustra como os sarcomas de mama induzidos por radiação podem ser de difícil diagnóstico e como o tratamento postergado pode exigir uma cirurgia de grande porte com maior morbidade. Estar ciente dessa condição pode melhorar o prognóstico do paciente.
Palavras-chave: sarcoma; neoplasias da mama; neoplasias induzidas por radiação; segunda neoplasia primária; relatos de casos.
RESUMEN
Introducción: El sarcoma de mama es una forma rara de cáncer que surge del tejido conectivo y comprende menos del 5% de todos los sarcomas. El sarcoma pleomórfico indiferenciado (SPI) de la mama es un subtipo raro y agresivo de sarcoma inducido por radiación que puede surgir en pacientes después de un tratamiento conservador del cáncer de mama. El diagnóstico es un desafío y, a menudo, se retrasa debido a la baja incidencia, el largo período de latencia, los hallazgos de imagen inespecíficos y las dificultades en la detección clínica e histológica. Informe del caso: Una paciente de 56 años fue diagnosticada de cáncer de mama triple negativo en estadio inicial en 2013 y se sometió a un tratamiento conservador para el cáncer de mama. A los cinco años de seguimiento desarrolló mastalgia y endurecimiento mamario, y tras mamografía y ecografía sin lesiones sospechosas, se realizó una resonancia magnética, que mostró una masa altamente sugestiva de malignidad de 8,0 cm. con invasión de la pared torácica. El estudio anatomopatológico de la lesión mostró un tumor de células fusiformes maligno, negativo para pancitoqueratina y para la mayoría de los marcadores inmuno-histoquímicos, lo que sugería sarcoma, pero requirió un estudio de la pieza quirúrgica para descartar un carcinoma metaplásico. La paciente fue intervenida de mastectomía radical de Halsted, resección de la pared torácica anterior izquierda cubriendo segmentos de las 4ª y 5ª costillas y reconstrucción con malla sintética. El informe histopatológico de la pieza quirúrgica mostró UPS, con márgenes libres. Evolucionó con buena recuperación postoperatoria, permaneciendo en seguimiento con el equipo de mastología. Conclusión: El relato de caso ilustra cómo los sarcomas de mama inducidos por radiación pueden ser difíciles de diagnosticar y cómo el tratamiento tardío puede requerir una cirugía mayor con mayor morbilidad. Ser consciente de esta condición puede mejorar el pronóstico del paciente.
Palabras clave: sarcoma; neoplasias de la mama; neoplasias inducidas por radiación; neoplasias primarias secundarias; informes de casos.
INTRODUCTION
Radiation therapy (RT) may be used to treat breast cancer at almost every stage. It is an essential component of breast conserving therapy, in addition to being an effective way to reduce the risk of breast cancer recurrence after surgery, allowing control of the microscopic residual disease, as well as improved survival1. Despite the proven benefits, the appearance of neoplastic events is a recognized complication attributed to RT1.
The potential for the development of radiation-induced sarcomas (RIS) is increasing because of the growing popularity of breast conserving surgery followed by irradiation in the treatment of mammary carcinomas2. Breast sarcoma is a rare group of heterogeneous non-epithelial tumors that appear in the connective tissue within the breast and are associated with poor prognosis. Subtypes include angiosarcoma, leiomyosarcoma, liposarcoma, fibrosarcoma and undifferentiated pleomorphic sarcoma (UPS), formerly known as malignant fibrous histiocytoma3,4. The present case describes a UPS secondary to RT for breast cancer with discussion of diagnosis and management challenges. The study complied with Resolution number 466/20125 of the National Health Council and was initiated after approval by the Institutional Review Board of the National Cancer Institute (INCA), report number 5,336,710, CAAE 57603422.2.0000.5274 (submission for ethical review).
CASE REPORT
A 56 years-old woman, obese, diabetic, negative family history of cancer, was diagnosed in 2013 at INCA with a high grade invasive ductal carcinoma of no special type (IDC-NST) in the left breast, hormone receptors and HER-2 (human epidermal growth factor receptor-type 2) negative, Ki67 60%, clinical stage IA. The patient underwent breast conserving surgery and sentinel lymph node biopsy (SLNB), the 1.0 cm tumor had clear margins and metastatic-free cells lymph nodes. After surgery she was prescribed adjuvant chemotherapy (adriamycin/cyclophosphamide), 21 sessions of radiotherapy and hormone therapy.
After 5 years of follow-up, the patient complained of pain and induration of the left breast; physical examination, mammogram and ultrasound (US) were performed, revealing changes attributed to the previous therapy. In addition to the induration (Figure 1), she presented chest pain with restriction of the arm movement and no suspicious axillary lymph nodes. A new mammogram revealed benign findings (BI-RADS® 2).
|
|
|
Figure 1. Alteration in left breast morphology, which can be confused with post-surgical aspect |
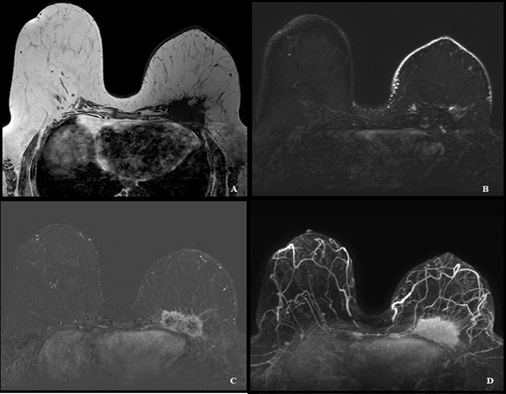
As there was clinical-radiologic disagreement, a 1.5 Tesla breast magnetic resonance imaging (MRI) was performed and showed an irregular, spiculated, contrast-enhanced mass, invading the chest wall, including the 4th and 5th left ribs, measuring 8.0x7.0x4.5cm, in the posterior third of the left breast, BI-RADS® 5 (highly suggestive of malignancy) (Figure 2).
|
|
|
Figure 2. MRI BI-RADS® 5. A) Hypointense mass at T1-weighted. B) Edema and thickening skin, which may represent post-surgical and post-actinic changes on the left breast. Hypointense mass in T2-weighted. C) Mass in the left breast showing heterogeneous contrast enhancement. Some areas do not impregnate contrast and may represent a necrotic component. D) Maximal intensity projection (MIP) image from contrast-enhanced MRI shows an irregular and spiculated mass |
Afterwards, an MRI-directed (“Second Look”) US was performed to guide a histopathological study, corresponding to hypoechoic, irregular, indistinct mass, no significant flow on Doppler, of a posterior location only possible to be observed in the vicinity of the left anterior axillary line (AAL).
Through a core needle biopsy, 5 good samples were obtained, revealing a spindle cells malignant tumor, hormone receptors and HER-2 negative, Ki67 80%, pan cytokeratin [AE1/AE3] negative, CK5/6 negative, p63 weakly positive, suggesting sarcoma, but requiring study of surgical specimen to exclude metaplastic carcinoma. In clinical staging, head, chest, abdomen and pelvis computed tomography scan did not show metastasis.
The patient underwent Halsted radical mastectomy, full-thickness left anterior chest wall resection contemplating segments of the 4th and 5th ribs and reconstruction with synthetic mesh (Figure 3). The surgical specimen evidenced an UPS, measuring 8.0 cm and infiltrating skeletal muscles and ribs, clear margins and 13 tumor free axillary lymph nodes. In the postoperative, the patient had seroma, which was solved after 3 punctures, and remained in follow-up without disease recurrence or complication for 1 and a half years at the end of the data collection period.
|
|
|
Figure 3. Surgical specimen of Halsted radical mastectomy and resection of the chest wall |
DISCUSSION
The case report presents a patient diagnosed with early-stage breast cancer that was treated with conservative surgery and radiation therapy and in a short-term follow-up developed a rare second primary neoplasm caused by the treatment of the first one. It was diagnosed as a breast sarcoma which required another surgical intervention, this time more aggressive but with satisfactory disease control.
Breast sarcomas can occur as a primary tumor and as a secondary form associated with a history of radiation therapy. Some authors6 describe UPS as the most common histopathological type6, others as angiosarcomas3,7; nevertheless, sarcomas following irradiation of breast cancer are rare and cumulative incidence is about 0.2% in 10 years8. They occur predominantly in 45-50 years old patients9. The average time for the development of the disease is about 10 years after radiation exposure, but varies between 6 months and 20 years10,11.
Risk factors besides previous radiotherapy are difficult to determine6. Patients who underwent radiotherapy as an initial treatment for breast carcer had until 16-fold increased risk of sarcomas, mainly angiossarcomas10. In addition, possible predisposing factors are genetic mutations (BRCA, TP 53), radiation in the chest wall/breast and the use of alkylating antineoplastic agent4,7, which, in this case, it was cyclophosphamide.
Pathogenesis of RIS, including UPS, is poorly understood. Genetic alterations and lesions are proposed mechanisms for radiation-induced tumor genesis in normal tissues8,12. RIS incidence is related to radiotherapy dose, occurring usually in patients that received around 60 – 80 Gray (Gy) and the minimum dose associated to RIS development was 10 Gy4,6. Establishing a causal relationship between the diagnosis of sarcoma and radiation therapy can be challenging. Cahan et al.13 established Cahan’s criteria in 1948, which were used to define a RIS. They are currently being used as the standard for demonstration of radio-induced malignancies.
The criteria define that evidence of an initial malignant tumor is needed, different than suspected RIS; the sarcoma must develop in an area that has been previously irradiated and around 4 years between the diagnosis of two malignancies, considering that sarcoma is the second one.
Diagnosis radiation-induced UPS can be challenging, first because the tumor is usually asymptomatic, and second, the post-radiation aspect of the breast tissue turns physical examination less sensitive3. Breast sarcomas most commonly manifest as a large, painless, mobile mass (mean diameter of 3 cm, reaching up to 30 cm), with rapid enlarging. Bilateral and axillary involvement are rarely described9,14,15.
The initial assessment is similar to the investigation of any suspicious mass in the breast: mammography, US and, in specific cases, MRI2. However, findings of UPS on imaging exams can be hard to notice due to typical post-surgical artifacts.
The sonographic appearance depicts usually nonhomogeneous and hypoechogenic mass, with areas of necrosis. The case reported has no expression on mammography, presenting changes due to therapy that may have made perception difficult for subtle findings and mammographic positioning tough, without ensuring that most of the tissue was included. In this patient, the posterior mass was only possible to be observed in the AAL, highlighting the importance of always looking at the entire breast, which extends vertically from the infraclavicular region to the inframammary fold and horizontally from the middle axillary line to the sternal region. MRI is considered better than mammography and ultrasound in characterizing and determining the extent of the disease over mammography and US. Also, MRI can be useful in identifying any residual disease following excisional procedure and guiding treatment planning.
Sarcoma’s diagnosis in patients who have undergone BCT is just as other mesenchymal tumors, typically performed through core needle biopsy. UPS is typically negative for most immuno-histochemical (IH) markers.
Metaplastic carcinoma is a differential diagnosis, as the morphology is similar; this is an undifferentiated, heterogeneous tumor, containing ductal carcinoma cells that may be mixed with other cell lineage, as spindle cells, squamous cells, or other mesenchymal origins. IH for metaplastic carcinoma should express at least one marker such as keratin or myoepithelial markers, although, as in this case, the final diagnosis comes only with the surgical specimen.
The prognosis for post radiation sarcomas is generally poor, with a 5-year survival rate of 27%-36% and has a high local rate of recurrence and metastasis3. Surgical intervention is a standard treatment for individuals who have not yet developed distant metastasis, and complete resection is crucial for a favorable long-term prognosis. Breast sarcomas typically do not spread to the lymph nodes, and as such, there is no evidence to suggest that a lymph node dissection improves the prognosis. Therefore, this procedure is not typically performed16.
Currently, the standard treatment of breast UPS consists in surgical resection with clear margins. Although mastectomy is often necessary, lumpectomy with clear margins may not negatively impact the outcome, and SLNB is not typically needed. Radiation therapy is often recommended for tumors that are large or for those that were not completely removed during surgery, presenting microscopically positive margins (R1) or even macroscopically residual disease (R2). Chemotherapy may not be very effective but tend to be prescribed in similar patients and in unresectable tumors. Therefore, the best treatment plan for each patient should be determined through a multidisciplinary approach, as there is no standard treatment protocol but a decision considering known prognostic factors and the surgery’s outcome3.
CONCLUSION
Radiation-induced breast UPS is a rare radiation-induced breast sarcoma. This case report intended to show how diagnosis can be difficult due to the resemblance to benign changes in breast tissue in the post-irradiated area. Therefore, the treatment and prognosis of the patient can be affected. Being aware of this diagnostic hypothesis can improve the clinical evolution and morbidity making this complication less harmful.
ACKNOWLEDGMENTS
To Shirley Moreira Burburan for critical review.
CONTRIBUTIONS
Tainara Rodrigues Miranda and Marie Nathalie Chenu contributed substantially to the study design, analysis and/or interpretation of the data, wording and/or critical review. Camila de Carvalho Figueiredo, Marcelo Morais Barbosa and Patricia Chaves de Freitas Campos Jucá contributed to the wording and/or critical review. All the authors approved the final version for publication.
DECLARATION OF CONFLICT OF INTERESTS
There is no conflict of interest to declare.
FUNDING SOURCES
None.
REFERENCES
1. Chansakul T, Lai KC, Slanetz PJ. The postconservation breast: part 2, imaging findings of tumor recurrence and other long-term sequelae. AJR Am J Roentgenol. 2012;198(2):331-43. doi: https://doi.org/10.2214/AJR.11.6881
2. Cesare A, Fiori E, Burza A, et al. Malignant fibrous histiocytoma of the breast. report of two cases and review of the literature. Anticancer Res [Internet]. 2005 [cited 2022 Feb 10];25(1B):505-8. Available from: https://ar.iiarjournals.org/content/25/1B/505.long
3. Kong J, Shahait AD, Kim S, et al. Radiation-induced undifferentiated pleomorphic sarcoma of the breast. BMJ Case Rep. 2020;13(2):e232616. doi: https://doi.org/10.1136/bcr-2019-232616
4. Kirova YM, Vilcoq JR, Asselain B, et al. Radiation-induced sarcomas after radiotherapy for breast carcinoma: a large-scale single-institution review. Cancer. 2005;104(4):856-63. doi: https://doi.org/10.1002/cncr.21223
5. Conselho Nacional de Saúde (BR). Resolução nº 466, de 12 de dezembro de 2012. Aprova as diretrizes e normas regulamentadoras de pesquisas envolvendo seres humanos. Diário Oficial da União, Brasília, DF. 2013 jun 13; Seção 1:59.
6. Sheth GR, Cranmer LD, Smith BD, et al. Radiation-induced sarcoma of the breast: a systematic review. Oncologist. 2012;17(3):405-18. doi: https://doi.org/10.1634/theoncologist.2011-0282
7. Whorms DS, Fishman MDC, Slanetz PJ. Mesenchymal lesions of the breast: what radiologists need to know. AJR Am J Roentgenol. 2018;211(1):224-33. doi: https://doi.org/10.2214/AJR.17.19020
8. Taghian A, de Vathaire F, Terrier P, et al. Long-term risk of sarcoma following radiation treatment for breast cancer. Int J Radiat Oncol Biol Phys. 1991;21(2):361-7. doi: https://doi.org/10.1016/0360-3016(91)90783-z
9. Matsumoto RAEK, Hsieh SJK, Chala LF, et al. Sarcomas of the breast: findings on mammography, ultrasound, and magnetic resonance imaging. Radiol Bras. 2018;51(6):401-6. doi: https://doi.org/10.1590/0100-3984.2016.0141
10. Huang J, Mackillop WJ. Increased risk of soft tissue sarcoma after radiotherapy in women with breast carcinoma. Cancer. 2001;92(1):172-80. doi: https://doi.org/10.1002/1097-0142(20010701)92:1<172::aid-cncr1306>3.0.co;2-k
11. Travis EL, Kreuther A, Young T, et al. Unusual postirradiation sarcoma of chest wall. Cancer. 1976;38(6):2269-73. doi: https://doi.org/10.1002/1097-0142(197612)38:6<2269::aid-cncr2820380613>3.0.co;2-7
12. Singh GK, Yadav V, Singh P, et al. Radiation-induced malignancies making radiotherapy a “two-edged sword”: a review of literature. World J Oncol. 2017;8(1):1-6. doi: https://doi.org/10.14740/wjon996w
13. Cahan WG, Woodard HQ, Higinbotham NL, et al. Sarcoma arising in irradiated bone: report of eleven cases. 1948. Cancer. 1998;82(1):8-34. doi: https://doi.org/10.1002/(sici)1097-0142(19980101)82:1<8::aid-cncr3>3.0.co;2-w
14. Cesa LS, Filippini BC, Tusset LC, et al. A clinical-pathological correlation in the diagnosis of breast sarcoma. Mastology, 2017;27(2):144-7. doi: https://doi.org/10.5327/Z2594539420170000163
15. Feder JM, de Paredes ES, Hogge JP, et al. Unusual breast lesions: radiologic-pathologic correlation. Radiographics. 1999;19(Suppl 1):S11-S26. doi: https://doi.org/10.1148/radiographics.19.suppl_1.g99oc07s
16. Yamazaki H, Shimizu S, Yoshida T, et al. A case of undifferentiated pleomorphic sarcoma of the breast with lung and bone metastases. Int J Surg Case Rep. 2018;51:143-6. doi: https://doi.org/10.1016/j.ijscr.2018.07.049
Recebido em 16/1/2023
Aprovado em 11/4/2023
Scientific-Editor: Anke Bergmann. Orcid iD: https://orcid.org/0000-0002-1972-8777
![]()
Este é um artigo publicado em acesso aberto (Open Access) sob a licença Creative Commons Attribution, que permite uso, distribuição e reprodução em qualquer meio, sem restrições, desde que o trabalho original seja corretamente citado.
©2019 Revista Brasileira de Cancerologia | Instituto Nacional de Câncer | Ministério da Saúde