Mixed-Cell Type Choroidal Melanoma in a Middle-Aged Woman
Melanoma de Coroide do Tipo Misto em uma Mulher de Meia-Idade
Melanoma Coroideo de Tipo Mixto en una Mujer de Mediana Edad
doi: https://doi.org/10.32635/2176-9745.RBC.2023v69n2.3890
Mirelly Aparecida Nolasco Frinhani1; Rebeca Alves Pestana2; Giuliane Stefane Braga Dantas3; Matheus Alves Bastianello4; Filipe de Carvalho Emery Ferreira5; Karina Coutinho Altoé6; Marcielle Grobério Franzin7; Clairton Marcolongo-Pereira8; Orlando Chiarelli-Neto9
1-4,6-9Centro Universitário do Espírito Santo (Unesc). Colatina (ES), Brazil. E-mails: mirelly_nolasco@hotmail.com; rebeca-alves@outlook.com; giulianestefane@hotmail.com; matheusbastianello@hotmail.com; karinacoutinho.a@gmail.com; marcigroberio@gmail.com; clairton.marcolongo@terra.com.br; orlandobqi@yahoo.com.br. Orcid iD: https://orcid.org/0000-0001-5873-5913; Orcid iD: https://orcid.org/0000-0003-4700-1249; Orcid iD: https://orcid.org/0000-0002-1289-3083; Orcid iD: https://orcid.org/0000-0003-2920-7163; Orcid iD: https://orcid.org/0000-0002-3092-5309; Orcid iD: https://orcid.org/0000-0003-2325-1382; Orcid iD: https://orcid.org/0000-0002-5593-3110; Orcid iD: https://orcid.org/0000-0002-8685-1185
5Faculdade de Medicina, Universidade de Vila Velha (UVV). Vila Velha (ES), Brazil. E-mail: fiemerymed@gmail.com. Orcid iD: https://orcid.org/0009-0001-9071-2137
Corresponding authors: Clairton Marcolongo-Pereira and Orlando Chiarelli-Neto. Av. Fioravanti Rossi, 2930 – Martinelli. Colatina (ES), Brazil. CEP 29703-858. E-mails: clairton.marcolongo@terra.com.br; orlandobqi@yahoo.com.br
ABSTRACT
Introduction: Melanomas are malignant neoplasms that occur in various anatomical sites, including the eye. Ocular melanomas account for 5% of all melanomas and are mainly described in Caucasian and older individuals. This study describes the clinical and pathological characteristics of uveal (choroid) melanoma in a Caucasian patient. Case report: A 41-year-old Caucasian female patient, brown eyes, without history of ophthalmological diseases or family history of cancer experienced pain and loss of visual acuity in the left eye. On clinical examination, an increase of ocular pressure was detected. Ultrasound showed a mushroom-like neoformation. Moreover, magnetic resonance imaging showed a mass with spontaneous hypersignal on T1-weighted images, intense gadolinium enhancement, and marked hyposignal on T2-weighted images. The patient was referred to the Oncology Ophthalmology department for enucleation due to suspected uveal melanoma. Anatomopathological analysis revealed a blackened mass in the eyeball. Histologically, the mass comprised spindle cells (50%) and epithelioid cells (50%). A diagnosis of choroidal melanoma was established based on the identification of ophthalmoscopic, imaging, and histological characteristics of the tumor. Conclusion: Choroidal melanomas usually occur in males, clear-eyed, and older individuals. A wide variety of ocular lesions may mimic choroidal melanoma, which should be included in the differential diagnosis of choroidal nevus and peripheral hemorrhages.
Key words: choroid neoplasms; melanoma; eye enucleation; eye pain.
RESUMO
Introdução: Melanomas são neoplasias malignas que ocorrem em vários sítios anatômicos, incluindo o olho. Os melanomas oculares correspondem a 5% de todos os melanomas e são descritos principalmente em indivíduos caucasianos e idosos. Este estudo descreve as características clinicopatológicas de um caso de melanoma uveal (coroide) em um paciente caucasiano. Relato do caso: Paciente, sexo feminino, 41 anos, caucasiana, olhos castanhos, sem antecedentes de doenças oftalmológicas e sem história familiar de câncer, com queixa de dor e perda da acuidade visual no olho esquerdo. No exame clínico, observou-se aumento da pressão ocular. O ultrassom revelou neoformação com aspecto de cogumelo, e a ressonância magnética, massa com hipersinal espontâneo em T1, intenso realce pelo gadolínio e marcado hipossinal em T2. A paciente foi encaminhada para cirurgia de enucleação em razão da suspeita de melanoma uveal. Foi realizada análise anatomopatológica que evidenciou massa enegrecida no interior do globo ocular. Histologicamente, a massa era constituída por 50% de células fusiformes e 50% de células epitelioides. O diagnóstico de melanoma de coroide baseou-se nas características oftalmoscópicas, imaginológicas e histológicas do tumor. Conclusão: Melanomas de coroide geralmente ocorrem em pacientes do sexo masculino, de olhos claros e idosos. Alerta-se que uma grande variedade de lesões oculares pode se assemelhar ao melanoma de coroide e este deve ser considerado no diagnóstico diferencial de nevo de coroide e hemorragias periféricas.
Palavras-chave: neoplasias da coroide; melanoma; enucleação ocular; dor ocular.
RESUMEN
Introducción: Los melanomas son neoplasias malignas que se presentan en varios sitios anatómicos, incluido el ojo. Los melanomas oculares representan el 5% de todos los melanomas y se describen principalmente en individuos caucásicos y de mayor edad. Este estudio describe las características clínicas y patológicas del melanoma uveal (coroides) en un paciente caucásico. Informe del caso: Paciente femenino de 41 años, caucásica, ojos marrones, sin antecedentes de enfermedades oftalmológicas y sin antecedentes familiares de cáncer, que consulta por dolor y pérdida de agudeza visual en el ojo izquierdo. En el examen clínico se observó aumento de la presión ocular. La ecografía mostró una neoformación con aspecto de hongo y la resonancia magnética mostró una masa con hiperseñal espontánea en T1, realce intenso de gadolinio y marcada hiposeñal en T2. La paciente fue remitida para cirugía de enucleación por sospecha de melanoma uveal. Se realizó análisis anatomopatológico, el cual mostró una masa ennegrecida en el interior del globo ocular. Histológicamente, la masa constaba de un 50 % de células fusiformes y un 50 % de células epitelioides. El diagnóstico de melanoma de coroides se basó en las características oftalmoscópicas, imagenológicas e histológicas del tumor. Conclusión: Los melanomas coroideos generalmente ocurren en pacientes masculinos, de ojos claros y de edad avanzada. Se advierte que una amplia variedad de lesiones oculares puede asemejarse al melanoma coroideo, y esto debe incluirse en el diagnóstico diferencial de nevus coroideo y hemorragias periféricas.
Palabras clave: neoplasias de la coroides; melanoma; enucleación del ojo; dolor ocular.
INTRODUCTION
Melanomas are malignant neoplasms that arise from neoplastic melanocytes. They can occur in various anatomical sites, including the eye1. In the eye, this tumor occurs mainly in the uvea and conjunctiva. Ocular melanomas represent approximately 5% of all melanomas2 and are mainly found in older Caucasian individuals1. In Brazil, an average of two thousand cases/million/year of this tumor has been reported2,3.
The main clinical manifestations in patients with this neoplasm comprise ocular dysfunction characterized by metamorphopsia, visual field loss, floaters, photopsia, and blurred vision1. However, 30% of the patients with uveal melanoma were found to be asymptomatic1. The suggestive diagnosis of uveal melanoma is based on routine clinical and ophthalmic examinations2. Ultrasonography, computed tomography, and magnetic resonance imaging could also contribute to determine the diagnosis. However, definitive diagnosis should be based on histological examination of the eye tissues2.
This study aimed to describe the clinicopathological features of a case of uveal (choroid) melanoma in a middle-aged woman in Brazil’s Southeast State of Espírito Santo.
The Institutional Review Board of “Centro Universitário do Espírito Santo – Unesc” approved the study, CAAE (Submission to Ethical Review) 64814822.4.0000.5062, report number 5,747,064.
CASE REPORT
A 41-year-old Caucasian female patient (phototype II - skin burns easily and tans minimally, brown eye, and social drinker) experienced loss of visual acuity with eye pain, reporting the use of sunglasses. The patient denied smoking and had no history of ophthalmological diseases or family history of cancer. She visited an ophthalmologist approximately one month after symptom onset.
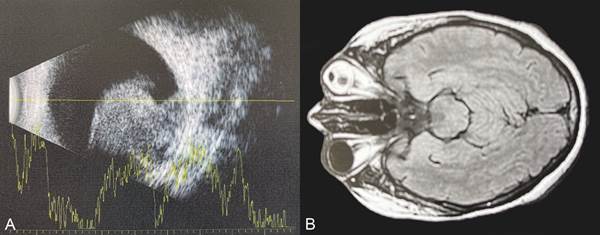
Ophthalmic examination revealed altered fundoscopy findings and preserved ocular motility. Intraocular pressure (IOP) was 12 mmHg in the right eye and 45 mmHg in the left eye. Ultrasonography of the left eye showed an elevated lesion with internal growth of the eyeball, characteristic of a heterogeneous mass, with mushroom-like appearance, cupuliform, in an advanced stage (Figure 1A).
The patient was referred to the Oncology Ophthalmology Department with a suspected uveal melanoma for diagnostic confirmation. Magnetic resonance imaging showed a vegetative lesion inside the left eyeball, measuring about 1.1 x 1.2 cm (base x height) in a mushroom-like shape, showing spontaneous hypersignal on T1-weighted sequences, intense enhancement by gadolinium, and marked hyposignal on T2-weighted images. There was also vitreous humor with hypersignals on fluid attenuated inversion recovery and an intermediate signal on T1-weighted images. The base of the tumor was in the posteroinferior and medial regions of the eyeball contiguous with the papilla. No signs of optic nerve invasion were observed (Figure 1B).
|
|
|
Figure 1. A. Ultrasonography of the left eye portraying a solid heterogeneous lesion with a mushroom-like appearance. B. Magnetic resonance imaging of the orbits showing a vegetating lesion with spontaneous hypersignal on T1-weighted images with intense gadolinium enhancement
|
Due to the clinical and imaging characteristics of the lesion, the patient was scheduled for urgent enucleation with implant insertion.
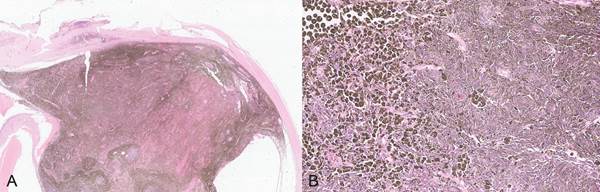
The excised eye was sent to anatomopathological analysis. Macroscopically, the eyeball measured 2.4 cm at the anteroposterior and 2.3 cm at the laterolateral ends. When excised, a blackened and soft mass measuring approximately 1.2 x 1.0 cm was noticed. Histologically, neoplastic proliferation was observed in the posterior portion of the choroid, which infiltrated the retina and partially extended into the sclera without extraocular extension. The intrascleral tumor extended to the posterior portion between the equatorial region and the ciliary body and measured 12.7 x 9.7 mm (basal diameter × thickness). The neoplasm had a solid pattern with diffuse pigmentation consisting of epithelioid cells (50%) and spindle cells (50%), indicating a mixed pattern (Figures 2A and 2B). There were one-two mitotic figures in 40 high-power fields and 20% of the tumor area was necrotic.
|
|
|
Figure 2. A. Dense non-encapsulated cell proliferation located in the posterior portion of the choroid infiltrating the retina. Hematoxylin and Eosin (HE), obj.10x B. There is proliferation of fusiform cells arranged in bundles in different directions and round cells with solid arrangement and moderate pleomorphism. The cytoplasm of the cells is full of brown granules. HE, obj.40x
|
The excised specimen was sent for immunohistochemistry and immunostaining for HMB45 and Melan A antibodies.
Ultrasonography of the entire abdomen was performed to identify metastases; however, no alterations were found.
DISCUSSION
The diagnosis of choroidal melanoma was based on ophthalmoscopic, imaging, and histological characteristics of the tumor. Melanomas arise when abnormal, uncontrolled, and autonomously proliferated melanocytes develop due to intrinsic (genetic) and/or extrinsic (epigenetic/environmental) factors4. In general, whereas mutations in the BRAF and NRAS genes have been shown to be present in most of the cutaneous melanoma, GNAQ and GNA11 mutations are involved in the development of uveal melanomas5. Enucleation is the most recommended treatment, because it is a malignant neoplasm, unnecessary enucleation due to errors in diagnosis of choroidal melanoma has become rare in specialized oncology centers5. However, in non-specialized centers, this error persists. It has been reported that approximately 30% of patients referred to specialized ocular oncology services with a diagnosis of choroidal melanoma had wrong diagnoses6.
The diagnosis of choroidal melanoma is based on detailed evaluation of the fundus with ophthalmoscopy, associated with imaging tests, such as ultrasound, tomography, and magnetic resonance imaging. Ultrasonography helps to define the extension, size, and shape of the tumor1. On computed tomography, uveal melanoma appears as a hyperdense structure with mild to moderate contrast. In addition, on magnetic resonance imaging, the lesion appears hyperintense on T1 - and hypointense on T2 - weighted sequences1.
Uveal melanoma can occur in the anterior and posterior tracts of the eye, affecting the iris, ciliary body, and choroid, with the latter being the most frequently affected by neoplasms1. This type of tumor tends to appear commonly in people aged over 70 years. However, it can affect individuals at any age and has already been described in adolescents, children, and newborns7.
It is noteworthy that uveal melanomas generally occur in individuals with light-colored eyes8 and are possibly associated with long-lasting exposure to ultraviolet (UV-B and UV-A) and visible radiation9,10. It has been mentioned that uveal melanoma was more incident in men11. Nevertheless, an epidemiological study in Brazil on the incidence of uveal melanoma found higher incidence of this type of tumor in women similar to the case described12. However, the difference in the proportion between men and women in the study was not very high.
The clinical presentation of choroidal melanoma varies. Most patients develop blurred vision and loss of visual acuity without pain13. Pain may be the only symptom observed in patients with uveal melanoma and is possibly related to glaucoma, inflammation, or necrosis8. Furthermore, uveal melanoma should be considered as a differential diagnosis in patients with unexplained headaches with or without ocular pain.
Histologically, the patient's tumor was classified as a mixed tumor (50% of spindle cells and 50% of epithelioid cells). Histological examination of the tumor is fundamental to help the oncologist to identify the patient’s prognosis. The morphological characteristics of the neoplasm, such as cell type, growth pattern, and proliferative activity (mitotic index or proliferation rate by immunohistochemistry: Ki67), may indicate worse or better prognosis9. Several studies have established that uveal spindle cell melanoma had the best prognosis, mixed-cell melanoma had an intermediate prognosis, epithelioid cell melanoma showed the worst prognosis14. Furthermore, the increase of the number of mitoses observed under the 40 highest power fields (HPS) was directly associated with a higher mortality rate. A six-year mortality rate has been estimated at 16% for 0 mitoses/40HPS, 23% for 1 mitoses/40HPS, 40% for 2-4 mitoses/40HPS, 47% for 5-8 mitoses/40HPS, and 56 % for 9-48 mitoses/40 HPS14. In this case, 1-2 mitotic figures were observed in 40 high-power fields, indicating a good prognosis.
Immunohistochemistry can be used to confirm diagnosis of choroidal melanomas, particularly when pigmentation is not amelanotic. Patients with choroidal melanomas exhibit positive immunostaining for antigens HMB45, Melan-A, MITF, tyrosinase, vimentin, and SOX1010. Differently from what is observed in cutaneous melanomas, the S-100 protein shows variable immunostaining in choroidal melanomas15. HMB45 antigen, tyrosinase, Melan-A, SOX10 and MITF are the best immunomarkers for detecting choroidal melanomas, as they show strong staining in different histological types described for this tumor16. Positive immunostaining for HMB45 and Melan A antibodies was observed in the patient, supporting the diagnosis of melanoma.
A wide variety of ocular lesions may mimic choroidal melanomas. The main differential diagnoses of this tumor are choroidal nevus, exudative peripheral hemorrhage, chorioretinopathy, congenital hypertrophy of the retinal pigmented epithelium, hemorrhagic retinal detachment or pigmented epithelium, choroidal hemangioma, and age-related macular degeneration1.
CONCLUSION
The diagnosis of choroidal melanomas can be challenging, and a wide variety of ocular lesions may mimic this neoplasm. Nevertheless, it is important to continue diagnostic investigation since the treatment and prognosis of the patient can be affected.
CONTRIBUTIONS
All authors contributed to the study design, wording, and critical review the manuscript. They approved the final version for publication.
DECLARATION OF CONFLICT OF INTERESTS
There is no conflict of interest to declare.
FUNDING SOURCES
This study was funded partially by Coordenação de Aperfeiçoamento de Pessoal de Nível Superior - Brasil (Capes) Code 001 and by Fundação de Amparo à Pesquisa e inovação do Espírito Santo (Fapes).
REFERENCES
1. Kaliki S, Shields CL. Uveal melanoma: relatively rare but deadly cancer. Eye (Lond). 2017;31(2):241-57. doi: https://doi.org/10.1038/eye.2016.275
2. Branisteanu DC, Bogdanici CM, Branisteanu DE, et al. Uveal melanoma diagnosis and current treatment options (Review). Exp Ther Med. 2021;22(6):1428. doi: https://doi.org/10.3892/etm.2021.10863
3. Calabria AC, Kempfer AV, Omizzolo JAE, et al. Melanomas primários de órbita: uma revisão narrativa da literatura. Soc Development. 2021;10(16): e103101623682. doi: https://doi.org/10.33448/rsd-v10i17.23682
4. Strashilov S, Yordanov A. Aetiology and pathogenesis of cutaneous melanoma: current concepts and advances. Int J Mol Sci. 2021;22(12):6395. doi: https://doi.org/10.3390/ijms22126395
5. Lange MJ, Razzaq L, Versluis M, et al. Distribution of GNAQ and GNA11 mutation signatures in uveal melanoma points to a light dependent mutation mechanism. PLoS One. 2015;10(9):e0138002. doi: https://doi.org/10.1371/journal.pone.0138002
6. Khan J, Damato BE. Accuracy of choroidal melanoma diagnosis by general ophthalmologists: a prospective study. Eye (Lond). 2007;21(5):595-7. doi: https://doi.org/10.1038/sj.eye.6702276
7. Tara S, Prabu R, Muralidhar V. Congenital uveal malignant melanoma- A rare case report. Am J Ophthalmol Case Rep. 2022;26:101539. doi: https://doi.org/10.1016/j.ajoc.2022.101539
8. Foti PV, Inì C, Broggi G, et al. Histopathologic and MR imaging appearance of spontaneous and radiation-induced necrosis in uveal melanomas: initial results. Cancers (Basel). 2022;14(1):215. doi: https://doi.org/10.3390/cancers14010215
9. Broggi G, Russo A, Reibaldi M, et al. Histopathology and genetic biomarkers of choroidal melanoma. Appl Sci. 2020;10(22):8081. doi: https://doi.org/10.3390/app10228081
10. Chalada M, Ramlogan-Steel CA, Dhungel BP, et al. The impact of ultraviolet radiation on the aetiology and development of uveal melanoma. Cancers (Basel). 2021;13(7):1700. doi: https://doi.org/10.3390/cancers13071700
11. Virgili G, Gatta G, Ciccolallo L, et al. Incidence of uveal melanoma in Europe. Ophthalmology. 2007;114(12):2309-15. doi: https://doi.org/10.1016/j.ophtha.2007.01.032
12. Lucena E, Goldemberg DC, Thuler LCS, et al. Epidemiology of uveal melanoma in Brazil. Int J Retina Vitreous. 2020;6(1):51. doi: https://doi.org/10.1186/s40942-020-00261-w
13. Shields CL, Manalac J, Das C, et al. Choroidal melanoma: clinical features, classification, and top 10 pseudomelanomas. Curr Opin Ophthalmol. 2014;25(3):177-85. doi: https://doi.org/10.1097/ICU.0000000000000041
14. Kaliki S, Shields CL, Shields JA. Uveal melanoma: estimating prognosis. Indian J Ophthalmol. 2015;63(2):93-102. doi: https://doi.org/10.4103/0301-4738.154367
15. Fernandes BF, Odashiro AN, Saraiva VS, et al. Immunohistochemical expression of melan-A and tyrosinase in uveal melanoma. J Carcinog. 2007;6:6. doi: https://doi.org/10.1186/1477-3163-6-6
16. Iwamoto S, Burrows RC, Kalina RE, et al. Immunophenotypic differences between uveal and cutaneous melanomas. Arch Ophthalmol. 2002;120(4):466-70. doi: https://doi.org/10.1001/archopht.120.4.466
Recebido em 17/3/2023
Aprovado em 3/5/2023
Scientific-Editor: Anke Bergmann. Orcid iD: https://orcid.org/0000-0002-1972-8777
![]()
Este é um artigo publicado em acesso aberto (Open Access) sob a licença Creative Commons Attribution, que permite uso, distribuição e reprodução em qualquer meio, sem restrições, desde que o trabalho original seja corretamente citado.
©2019 Revista Brasileira de Cancerologia | Instituto Nacional de Câncer | Ministério da Saúde