CASE REPORT
Metastasis of Pulmonary Carcinoma to the Breast: Case Report
Metástase de Carcinoma Pulmonar para Mama: Relato de Caso
Metástasis de Carcinoma Pulmonar a la Mama: Informe de Caso
doi: https://doi.org/10.32635/2176-9745.RBC.2023v69n3.4052
Flávio Roberto Garbelini de Oliveira1; Daniel Nunes Milani2; José Cândido Caldeira Xavier-Júnior3; Daniella Rezende Ferreira4; Tony Maronesi Bagio5; Fernanda Alvim Chrisostomo6
1Centro Universitário Católico Salesiano Auxilium (UniSALESIANO). Hospital Unimed. Liga Acadêmica de Pneumologia e Cirurgia Torácica (LAPCT). Araçatuba (SP), Brazil. E-mail: garbelin@terra.com.br. Orcid iD: https://orcid.org/0000-0003-0696-8752
2Hospital Unimed. Araçatuba (SP), Brazil. E-mail: oncomilani@gmail.com. Orcid iD: https://orcid.org/0000-0003-0650-1693
3UniSALESIANO. Instituto de Patologia de Araçatuba (IPAT). Araçatuba (SP), Brazil. E-mail: josecandidojr@yahoo.com.br. Orcid iD: https://orcid.org/0000-0003-0503-419X
4,5,6UniSALESIANO. LAPCT. Araçatuba (SP), Brazil. E-mails: daniellarferreira@gmail.com; tonymaronesi@gmail.com; fernanda_alvim@hotmail.com. Orcid iD: https://orcid.org/0000-0002-9457-7569; Orcid iD: https://orcid.org/0000-0002-9093-7125; Orcid iD: https://orcid.org/0000-0002-8595-4959
Corresponding author: Tony Maronesi Bagio. Rodovia Senador Teotônio Vilela, 3821 – Alvorada. Araçatuba (SP), Brazil. CEP 16016-500. E-mail: tonymaronesi@gmail.com
ABSTRACT
Introduction: Pulmonary carcinoma is the most prevalent cancer in the world, followed by breast cancer. It has high mortality rates in men and women mainly due to its ability to metastasize. Metastases from lung carcinoma to the breast are extremely rare. The first case described occurred in 1965 and since then there are few cases of this condition reported in the world medical literature. Case report: A 59-year-old woman who complained of low back pain in May 2017. The investigation revealed a metastatic site in the fifth vertebra of the lumbar spine with unknown origin. Six months later, a new lesion was found in the ninth vertebra of the thoracic spine. Immunohistochemistry showed positivity for cytokeratin 7 and TTF1 markers, confirming the hypothesis of lung carcinoma as the primary site. In March 2018, the patient evolved with a symptomatic nodule in the right breast on ultrasound and with positivity for TTF1 on immunohistochemical study, confirming the metastasis of lung carcinoma to the breast. Treated for two years until March 2020, when she presented multiple brain metastases. Patient had no therapeutic success and died. Conclusion: The difficulty in diagnosing lung carcinoma metastasis to the breast stands out, surgeons, clinicians and pathologists should consider this diagnosis, although rare.
Key words: lung neoplasms; breast neoplasms; neoplasm metastasis; case reports.
RESUMO
Introdução: O carcinoma pulmonar é o câncer mais prevalente no mundo, seguido pelo de mama. Apresenta altas taxas de mortalidade em homens e mulheres, principalmente em virtude da sua capacidade de metastatizar. As metástases do carcinoma de pulmão para a mama são extremamente raras. O primeiro caso descrito ocorreu em 1965 e, desde então, há poucos casos dessa condição relatados na literatura médica mundial. Relato do caso: Mulher, 59 anos, apresentou dor lombar em maio de 2017. A investigação revelou um local metastático na quinta vértebra da coluna lombar sem descobrir sua origem. Seis meses depois, uma nova lesão foi encontrada na nona vértebra da coluna torácica. A imuno-histoquímica mostrou positividade para os marcadores citoqueratina 7 e TTF1, confirmando a hipótese de carcinoma de pulmão como sítio primário. Em março de 2018, a paciente evoluiu com um nódulo sintomático na mama direita ao ultrassom e com positividade para TTF1 no estudo imuno-histoquímico, confirmando tratar-se de metástase de carcinoma de pulmão para a mama. Foi tratada por dois anos até março de 2020, quando apresentou múltiplas metástases cerebrais. A paciente não teve sucesso terapêutico e faleceu. Conclusão: Ressalta-se a dificuldade no diagnóstico de metástase de carcinoma de pulmão para a mama e alertar clínicos, cirurgiões e patologistas para que considerem esse diagnóstico, embora raro.
Palavras-chave: neoplasias pulmonares; neoplasias da mama; metástase neoplásica; relatos de casos.
RESUMEN
Introducción: Carcinoma de pulmón es el cáncer más prevalente del mundo, seguido del cáncer de mama. Presenta elevadas tasas de mortalidad en hombres y mujeres, debido principalmente a su capacidad de metástasis. Las metástasis del carcinoma de pulmón hacia la mama son extremadamente raras. El primer caso descrito fue en 1965 y, desde entonces, existen pocos casos de esta afección en la literatura médica de todo el mundo. Informe del caso: Mujer, 59 años, comenzó a experimentar dolor lumbar en mayo de 2017. La investigación reveló un foco metastásico en la quinta vértebra de la columna lumbar sin descubrir su origen. Seis meses después, se encontró una nueva lesión en la novena vértebra de la columna torácica. Inmunohistoquímica mostró positividad para los marcadores citoqueratina 7 y TTF1, confirmando la hipótesis de carcinoma de pulmón como localización primaria. En marzo de 2018, la paciente evolucionó con un nódulo sintomático en la mama derecha en la ecografía y con positividad para TTF1 en el estudio inmunohistoquímico, confirmando que se trataba de una metástasis de carcinoma pulmonar a la mama. Tratada durante dos años hasta marzo de 2020, cuando presentó múltiples metástasis cerebrales. La paciente no tuvo éxito terapéutico y falleció. Conclusión: Destacan la dificultad en el diagnóstico de metástasis de carcinoma pulmonar a la mama y alertar clínicos, cirujanos y patólogos para que consideren este diagnóstico, aunque poco frecuente.
Palabras clave: neoplasias pulmonares; neoplasias de la mama; metástasis de la neoplasia; informes de casos.
INTRODUCTION
The most recent Brazilian study estimates that between 2023 and 2025, there will be 704,000 new cases of cancer, 483,000 if non-melanoma skin cancer cases are excluded1,2. This is estimated to be the most incident, with 220,000 new cases (31.3%), followed by breast cancers with 74,000 (10.5%), prostate, with 72,000 (10.2%), colon and rectum, with 46,000 (6.5%)1. It is estimated that the most frequent types of cancer in men will be non-melanoma skin cancer, with 102,000 (29.9%) new cases, prostate, with 72,000 (21.0%), colon and rectum, with 22,000 (6.4%)1. In women, non-melanoma skin cancers, with 118,000 (32.7%), breast, with 74,000 (20.3%) and colon and rectum, with 24,000 (6.5%) will be the most frequent1.
In relation to global data, lung carcinoma has high mortality rates in men and women, mainly due to the fact that more than half of the cases are diagnosed in advanced stages of the disease3.
The four main histological types of lung carcinoma are adenocarcinoma, squamous cell carcinoma, small cell neuroendocrine carcinoma, and large cell neuroendocrine carcinoma1,2,4-6. In some cases there may be a combination of different histological types4,5.
Case reports in the literature on breast metastases from lung cancer are scarce, with the first case reported in history in 1965 in England7.
Metastases from lung cancer to the breast are extremely rare8. The literature show that extra-mammary metastases correspond to 0.4 to 1.3% of breast carcinomas. The most common tumors that metastasize to the breast are melanoma, lung cancer, renal cell carcinoma, and ovarian tumors8,9. Lung cancer accounts for 16 to 33% of all breast metastasis cases, with adenocarcinoma being the most common subtype8.
In the last 5 years, only six cases were found in the literature that showed metastasis of lung carcinoma to the breast, demonstrating the rarity of this condition10-12. Therefore, the purpose of this study is to report the case of a 59-year-old woman, who in 2017 was diagnosed with lung adenocarcinoma evolving to metastasis in the breast. The Institutional Review Board of “Centro Universitário Católico Salesiano Auxilium” approved the study (CAAE 52531121.6.0000.5379 (Submission for Ethical Review), report number 5,233,599) in compliance with Resolution 466/1213 of the National Health Council for research with human beings.
CASE REPORT
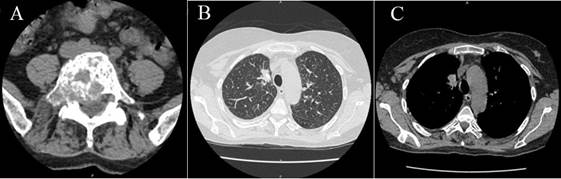
Female patient, 59 years old, white, married, with no history of smoking and no comorbidities, presented low back pain and loss of muscle strength in the right foot in May 2017. She sought an orthopedist and a neurosurgeon and was submitted to a CT scan of the lumbar spine where tumor infiltration of the fifth lumbar vertebra-L5 was found (Figure 1A). In June 2017, L5 lumbar spine arthrodesis and biopsy were performed with anatomopathological diagnosis of carcinoma metastasis exhibiting papillary architecture. An immunohistochemical study attempted to define the primary site of the neoplasm. Cytokeratin 7 was positive (clone: OV-TL 12/30) and negative for the other markers tested (cytokeratin 20, clone: Ks20.8; TTF1, clone: 8G7G3/1; mammaglobin, clone: 304-1A5; CDX2, clone: DAK-CDX2; WT1, clone: 6F-H2); therefore, it was not possible, at that moment, to define the primary site of the neoplasm.
Further investigations with chest tomography showed a nodular, spiculated image in the apical segment of the right upper lobe measuring 2.2 x 4.3 cm (Figure 1B, C). She was referred to the bronchoscopy department for flexible bronchoscopy. Transbronchial biopsy of the right upper lobe did not reveal any neoplasm. The patient evolved with pleural and pericardial effusion with negative cytological analysis and started chemotherapy treatment with Carboplatin and Paclitaxel, with later addition of Zoledronic acid for lung carcinoma with bone metastasis.
|
|
|
Figure 1. A) Tomography of lumbar spine showing osteolytic lesion of L5 (May 2017). B) and C) Chest CT scan showing nodular image with irregular contours and limits, spiculated, in the apical region of the right upper lobe, showing coarse calcifications inside, measuring 2.2 x 4.3 cm (June 2017) |
Six months later, the patient presented a new metastatic bone lesion in the ninth thoracic vertebra - T9, with the same microscopic characteristics as the first material, and underwent a new spinal arthrodesis and biopsy. In a new immunohistochemical study, with repetition of the markers previously tested and inclusion of two more markers, besides positivity for cytokeratin 7, there was positivity for TTF1 (clone: 8G7G3/1) and negativity for thyroglobulin (polyclonal) and GATA3 (clone L50-823), confirming the hypothesis of metastasis from lung carcinoma. Research of PD-L1 expression (clone 22C3), ALK expression (Clone: D5F3) and research of the EGFR mutation were performed in order to identify possible target therapy. The neoplastic cells were negative for PD-L1 and ALK, but a c.2236_2251delinsT;p.(Glu746_Thr751delinSer)(E746_Y751deilinsS) mutation was identified in exon 19 of the EGFR gene. The patient was followed up at the clinical oncology service, undergoing chemotherapy.
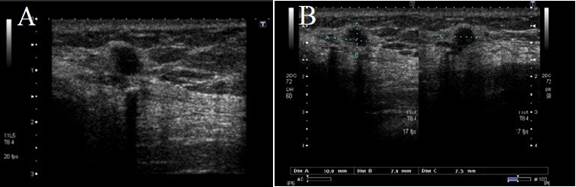
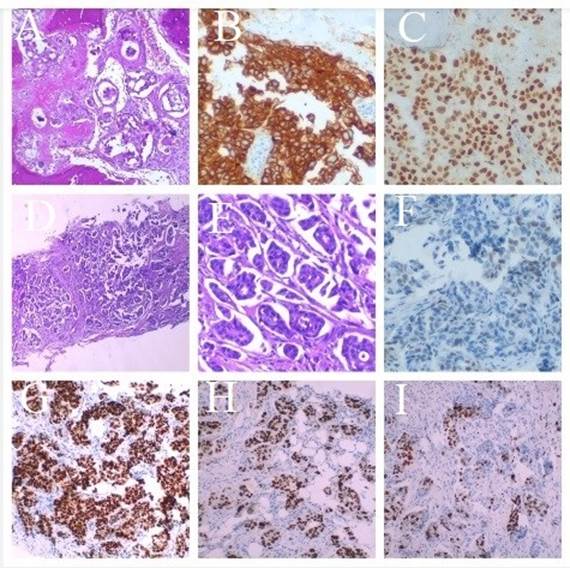
In March 2018, the patient presented with a right breast nodule on 7/8-hour radius, with the presence of peripheral hyperechogenicities, measuring 0.84 cm on breast ultrasound (Figure 2A, B), and was classified as BIRADS 4B. The nodule was submitted to core biopsy (Figure 3 A-D) from which ten fragments were removed. The anatomopathological examination identified malignant epithelial neoplasia with ductal architecture, without the presence of papillary arrangements. Moderate stromal desmoplasia and moderate inflammatory infiltrate were observed.
At the time the neoplasm was classified as invasive breast carcinoma of the non-special WHO/2012 type (Invasive Ductal Carcinoma without other specifications), histological grade (provisional) II/ moderately differentiated (Scarff-Bloom-Richardson modified by Elston and Ellis - tubular formation: score 2; nuclear grade: score 3; mitotic index: score 1; sum of scores: 6) without an "in situ" (intraductal) component.
|
|
|
Figure 2. Ultrasound showing noduliform image in right breast, predominantly anechoid at 7/8 hour, measuring 0.84 cm (June 2018) |
An immunohistochemical study for breast prognostic factors was requested (Figure 3 E-I). Given the finding of stronger positivity for progesterone receptor (clone: PgR 636; present in strong intensity in 50% of cells) in relation to estrogen receptor (clone: EP1, present in weak intensity in a focal manner) in association with the patient's history, the histogenesis of the neoplasm was also investigated. Negativity for mammaglobin and GATA3 and positivity for TTF1 were identified, confirming a metastasis of lung adenocarcinoma to the breast. The breast biopsy was submitted to EGFR mutation research, and a mutation in exon 19 plus a mutation (pT790M) in exon 20 were identified.
|
|
|
Figure 3. A) atypical epithelial cells arranged in cohesive clusters amidst bone trabeculae. HE. 100 X. B) diffuse staining. Cytokeratin 7 200x. C) diffuse positivity for TTF1 200x. D) breast biopsy. Note duct formation with artifact of retraction of adjacent stroma (very common finding in breast carcinomas). HE 40X. E) note the evident ductal formation characterized by atypical cells arranged around lumens. HE 200X. F) estrogen receptor exhibiting weak and focal positivity. Estrogen receptor 200X. G) strong and diffuse positivity for progesterone receptor. Progesterone receptor 100x. H) strong and diffuse positivity for TTF1. TTF1 100x. I) High cell proliferation rate. Ki67 100x |
The patient continued the chemotherapy treatment with Carboplatin, Paclitaxel, Erlotinib, Osimertinib and Docetaxel. The disease was stabilized by RECIST 1.1 criteria until March 2020, when she presented a disease progression in a primary lung lesion and multiple brain metastases detected on MRI of the skull. She underwent holocranial radiotherapy and subsequently fourth-line chemotherapy with two cycles, but without benefit, and died in April 2020 due to the progression of the neoplasms.
DISCUSSION
Extra-mammary metastases can spread via hematologic or lymphatic routes. The most common initial clinical manifestations are the appearance of solitary painless, palpable, and well circumscribed masses located more in the upper quadrant and do not present skin or nipple retraction2,11. However, lymphatic metastases can evolve with redness and swelling in the breast. In the case of lung neoplasms, the lymphatic route is more rare11.
Immunohistochemistry is crucial for the differential diagnosis between primary breast cancer and lung adenocarcinoma. There is no single marker in the literature with high sensitivity and specificity2. Thyroid Transcription Factor-1 (TTF1) is a well-established biomarker for lung carcinoma and is currently one of the most widely used to find the origin of the tumor. Current data indicate that 58% of non-small cell lung carcinomas that metastasize to the breast are TTF1 positive, while in cases of primary lung adenocarcinoma the positivity is 83%2,8. The estrogen receptor (ER) is present in up to 80% of breast malignancies and between 7.6 to 27.2% of lung adenocarcinoma cases. Progesterone receptor (PE) is expressed in 60% of breast cancers and between 1.6 and 51.4% of adenocarcinomas. Other markers can also be found such as GATA-3 (67-95% of breast cancers and up to 8% in adenocarcinoma) and Napsin A (84% lung adenocarcinoma versus 14.6% malignant breast neoplasm)2.
Another important element that must be highlighted in the case is the presence of the T790 mutation2. Epidermal growth receptor (EGFR) is a protein present in cells that plays a role associated with cell growth and survival2,8. It can present several mutations, one of them being the T790M mutation, which is related to resistance to EGFR tyrosine-kinase inhibitor therapy and disease progression. In the last five years, there have been no cases of lung carcinoma metastasizing to the breast with the presence of the T790M mutation in the world literature2.
CONCLUSION
A case of a 59-year-old patient diagnosed with adenocarcinoma of the lung metastasized to the breast and evolving to death was described. The differential diagnosis between primary breast carcinoma and malignant lung neoplasm is challenging, and the pathological study of the case is important. In addition, it is essential to correlate the data obtained in immunohistochemistry with the patient's clinical history in order to diagnose and treat the case as quickly and appropriately as possible. Clinicians, surgeons and pathologists should be aware that, even in the presence of morphological findings suggestive of ductal carcinoma, metastasis to the breast should be a possibility to be considered, although this is a rare occurrence.
CONTRIBUTIONS
All the authors contributed to the study design, wording of the manuscript, critical review of the literature and of the manuscript and approved the final version for publication.
DECLARATION OF CONFLICT OF INTERESTS
There is no conflict of interests to declare.
None.
REFERENCES
1. Instituto Nacional de Câncer. Estimativa 2023: incidência de câncer no Brasil [Internet]. Rio de Janeiro: INCA; 2022 [acesso 2023 jul 12]. Disponível em: https://www.inca.gov.br/sites/ufu.sti.inca.local/files//media/document//estimativa-2023.pdf
2. Mirrielees JA, Kapur JH, Szalkucki LM, et al. Metastasis of primary lung carcinoma to the breast: a systematic review of the literature. J Surg Res. 2014;188(2):419-31. doi: https://doi.org/10.1016/j.jss.2014.01.024
3. Silva LM, Silva GT, Bergmann A, et al. Impact of different patterns of metastasis in non-small-cell lung cancer patients. Future Oncol. 2021;17(7):775-82. doi: https://doi.org/10.2217/fon-2020-0587
4. Bray F, Ferlay J, Soerjomataram I, et al. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68(6):394-424. doi: https://doi.org/10.3322/caac.21492
5. Ferlay J, Colombet M, Soerjomatarm I, et al. Estimating the global cancer incidence and mortality in 2018: GLOBOCAN sources and methods. Int J Cancer. 2018;144(8):1941-53. doi: https://doi.org/10.1002/ijc.31937
6. Araujo LH, Baldotto C, Castro Júnior G, et al. Lung cancer in Brazil. J Bras Pneumol. 2018;44(1):55-64. doi: https://doi.org/10.1590/s1806-37562017000000135
7. Deeley TJ. Secondary deposits in the breast. Br J Cancer. 1965;19(4):738-43. doi: https://doi.org/10.1038/bjc.1965.85
8. Valenza C, Porta FM, Rappa A, et al. Complex differential diagnosis between primary breast cancer and breast Metastasis from EGFR-mutated lung adenocarcinoma: case report and literature review. Curr Oncol. 2021;28(5):3384-92. doi: https://doi.org/10.3390/curroncol28050292
9. Wang L, Wang SL, Shen HH, et al. Breast metastasis from lung cancer: a report of two cases and literature review. Cancer Biol Med. 2014;11(3):208-15. doi: https://doi.org/10.7497/j.issn.2095-3941.2014.03.007
10. Fujita T, Nishimura H, Kondo R, et al. Breast metastasis of pulmonary pleomorphic carcinoma: a case report. Surg Case Rep. 2017;3(1):25. doi: https://doi.org/10.1186/s40792-017-0302-6
11. Ota T, Hasegawa Y, Okimura A, et al. Breast metastasis from EGFR-mutated lung adenocarcinoma: a case report and review of the literature. Clin Case Rep. 2018;6(8):1510-6. doi: https://doi.org/10.1002/ccr3.1636
12. Zhao R, Xing J, Gao J. Breast metastasis of lung cancer after computed tomography-guided core needle biopsy: a case report. Front Surg. 2022;9:890492. doi: https://doi.org/10.3389/fsurg.2022.890492
13. Conselho Nacional de Saúde (BR). Resolução nº 466, de 12 de dezembro de 2012. Aprova as diretrizes e normas regulamentadoras de pesquisas envolvendo seres humanos. Diário Oficial da União, Brasília, DF. 2013 jun 13; Seção 1:59.
Recebido em 19/5/2023
Aprovado em 20/6/2023
Scientific-Editor: Anke Bergmann. Orcid iD: https://orcid.org/0000-0002-1972-8777
![]()
Este é um artigo publicado em acesso aberto (Open Access) sob a licença Creative Commons Attribution, que permite uso, distribuição e reprodução em qualquer meio, sem restrições, desde que o trabalho original seja corretamente citado.
©2019 Revista Brasileira de Cancerologia | Instituto Nacional de Câncer | Ministério da Saúde