Primary Malignant Melanoma of the Uterine Cervix: Rare Case Report
Melanoma Maligno Primário do Colo do Útero: Relato de um Caso Raro
Melanoma Maligno Primario del Cuello del Útero: Informe de un Caso Raro
https://doi.org/10.32635/2176-9745.RBC.2023v69n4.4410
Carlos Anselmo Lima1; Adriana Cardoso Batista Albuquerque2; Érika de Abreu Costa Brito3; Marcela Sampaio Lima4
1Universidade Federal de Sergipe (UFS), Hospital Universitário, Rede Ebserh. UFS, Programa de Pós-Graduação em Ciências da Saúde e Programa de Pós-Graduação Profissional em Gestão e Inovação Tecnológica em Saúde. Aracaju (SE), Brazil. E-mail: ca.lima01@gmail.com. Orcid iD: https://orcid.org/0000-0003-4269-7320
2,3,4UFS, Hospital Universitário, Rede Ebserh. UFS, Programa de Pós-Graduação em Ciências da Saúde. Aracaju (SE), Brazil. E-mails: drikascb@msn.com; kostabrito@hotmail.com; marcelasampaio@yahoo.com.br. Orcid iD: https://orcid.org/0000-0001-8046-7812; Orcid iD: https://orcid.org/0000-0003-0050-1799; Orcid iD: https://orcid.org/0000-0003-1738-4023
Corresponding author: Carlos Anselmo Lima. Rua Cláudio Batista 505 – Palestina. Aracaju (SE), Brazil. CEP 49060-676. E-mail: ca.lima01@gmail.com
ABSTRACT
Introduction: Primary cervical melanoma is a rare and often challenging diagnosis, particularly in the presence of amelanotic lesions, where confirmation should be made through immunohistochemical methods. Despite aggressive treatment, the prognosis for this disease is typically poor. Case Report: A 79-year-old woman with a history of vaginal bleeding from a malignant cervical lesion. Initially, colposcopy examination revealed an ulcerated lesion of the exocervix, and biopsy confirmed a malignant neoplasm. However, following a radical abdominal hysterectomy, histopathological examination displayed a malignant epithelioid neoplasm, confirmed a malignant melanoma of the cervix through immunohistochemical assays. The patient received adjuvant chemotherapy and radiation therapy, but eventually experienced recurrence and died. Conclusion: The present report assesses a patient with an uncommon diagnosis of cervical melanoma, which, despite aggressive treatment, had an unfavorable outcome. However, thorough skin surveillance should be performed to correctly diagnose it as primary.
Key words: cervix uteri; uterine cervical neoplasms; melanoma.
RESUMO
Introdução: O melanoma cervical primário é um diagnóstico raro e frequentemente desafiador, especialmente na presença de lesões amelanóticas, cuja confirmação deve ser feita por métodos imuno-histoquímicos. Apesar do tratamento agressivo, o prognóstico para essa doença costuma ser ruim. Relato do caso: Mulher, 79 anos, com histórico de sangramento vaginal decorrente de uma lesão cervical maligna. Inicialmente, a colposcopia revelou uma lesão ulcerada no exocérvix e a biópsia confirmou ser um tumor maligno. No entanto, após uma histerectomia abdominal radical, o exame histopatológico mostrou tratar-se de uma neoplasia maligna epitelioide, confirmada como um melanoma maligno do colo do útero por meio de exame imuno-histoquímico. A paciente recebeu quimioterapia adjuvante e radioterapia, mas eventualmente apresentou recorrência e veio a óbito. Conclusão: O presente relato avalia uma paciente com um diagnóstico incomum de melanoma cervical que, apesar do tratamento agressivo, teve um desfecho desfavorável. No entanto, uma vigilância cutânea minuciosa deve ser realizada para diagnosticá-lo corretamente como primário.
Palavras-chave: colo do útero; neoplasias do colo do útero; melanoma.
RESUMEN
Introducción: El melanoma cervical primario es un diagnóstico raro y a menudo desafiante, especialmente en presencia de lesiones amelanóticas, donde la confirmación debe hacerse mediante métodos inmunohistoquímicos. A pesar del tratamiento agresivo, el pronóstico de esta enfermedad suele ser malo. Informe del caso: Mujer, 79 años, con antecedentes de sangrado vaginal debido a una lesión cervical maligna. Inicialmente, el examen colposcópico reveló una lesión ulcerada del exocérvix y la biopsia confirmó que se trataba de una neoplasia maligna. Sin embargo, después de una histerectomía abdominal radical, el examen histopatológico mostró una neoplasia epitelioide maligna, confirmada como un melanoma maligno del cuello uterino mediante pruebas inmunohistoquímicas. La paciente recibió quimioterapia adyuvante y radioterapia, pero finalmente sufrió una recurrencia y falleció. Conclusión: El presente informe evalúa a una paciente con un diagnóstico poco común de melanoma cervical, que, a pesar del tratamiento agresivo, tuvo un resultado desfavorable. Sin embargo, para diagnosticarlo correctamente como primario, se debe realizar una vigilancia exhaustiva de la piel.
Palabras clave: cuello del útero; neoplasias del cuello uterino; melanoma.
INTRODUCTION
The diagnosis of primary melanoma in mucosal sites is uncommon, accounting for less than 4% of all melanoma cases. These lesions are primarily found in the oral cavity, esophagus, anus, conjunctiva, and vulvovaginal epithelium, and are difficult to diagnose due to the absence of melanin, a characteristic feature of cutaneous melanomas1.
Primary melanoma of the uterine cervix is an extremely rare condition, with only a few cases reported in the world literature2-4. Unlike non-cutaneous melanomas, primary cervical melanomas often present in advanced stages and have a more aggressive course, leading to a poorer prognosis5. Confirmatory diagnosis typically requires immunohistochemical assays, and staging tests are performed to assess the presence of metastasis6.
The purpose of this study is to report an unusual case of primary melanoma of the cervix, including its diagnosis, management, and follow-up until the patient's death. In compliance with the current legislation, the study was submitted, reviewed and approved by the Institutional Review Board of “Universidade Federal de Sergipe” CAAE (submission for ethical review) number 71636723.2.0000.5546 and approval report number 6,319,121, in compliance with Resolution 466/20127 of the National Health Council.
CASE REPORT
A 74-year-old Brazilian female of African descent presented with vaginal bleeding. Three days later, she was evaluated by a gynecologist who identified and performed a biopsy on a cervical lesion. The initial biopsy confirmed the diagnosis of squamous cell carcinoma of the cervix. Following this, one-month post-biopsy, the patient was admitted to the Oncologic Facility for a comprehensive gynecologic examination. The examination revealed a 4-cm cervical lesion that exhibited no invasion into the vagina or parametrium. Subsequent assessments including blood, urine, and cardiac tests, chest x-ray, and abdominal ultrasound were performed, ruling out any extra-uterine involvement. Based on clinical and imaging evaluations, the lesion was staged as FIGO (International Federation of Gynecology and Obstetrics, 20098) IB1.
Forty-four days after the initial symptoms, the patient underwent a radical abdominal hysterectomy with pelvic lymphadenectomy. Histopathological examination revealed a malignant 3.5 cm width, 1.4 cm deep epithelioid neoplasm, consisting of papillary and fusocellular areas, limited to the exocervix and negative pelvic lymph nodes, consistent with previously determined clinical staging. She had an uneventful post operative course.
Due to the diagnosis of an epithelioid neoplasm, immunohistochemistry (Table 1) was performed and revealed expression of the proteins S-100 (Figure 1) and Melan-A (Figure 2), indicating malignant melanoma. The lack of cutaneous lesions led to a final diagnosis of primary melanoma of the uterine cervix.
Following the processing of the surgical specimen and subsequent immunohistochemical analysis, there was a remarkable delay in reaching the final diagnosis. Eighty-two days post-surgery, the patient underwent adjuvant treatment comprising dacarbazine (D1-D3), carmustine (D1), and cisplatin (D1-D3) concurrently with external beam radiation (whole pelvic 45 Gy; 28 Fr/1.8 Gy), followed by brachytherapy (24 Gy at point C; 4 Fr/6 Gy). The patient did not experience any major complications during the adjuvant treatment, and extended granulocytopenia was prevented with filgrastim. Eleven months after completing brachytherapy, the patient was diagnosed with lung metastasis, peritoneal recurrence, and ascites, and succumbed to these conditions within two months.
Table 1. Immunohistochemical markers, melanoma of the uterine cervix
|
Antibodies |
Clone |
Result |
|
Cytokeratins – 40, 48, 50, 50.6 kDa |
AE1/AE3 |
Negative |
|
Protein p63 |
Dak-p63 |
Negative |
|
P16 (INK4) |
G175-405 |
Negative |
|
Cytokeratin 5/6 |
D5/16B4 |
Negative |
|
Protein S-100 |
Polyclonal |
Positive |
|
Melan A (MART-1) |
D5/16B4 |
Positive |
|
Desmin |
D33 |
Negative |
|
Myogenin |
F5D |
Negative |
|
Chromogranin A |
DAK-A3 |
Negative |

Figure 1. Immunohistochemical expression of protein S-100
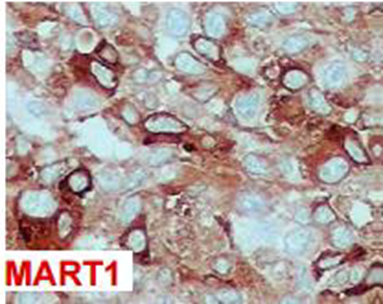
Figure 2. Immunohistochemical expression of MART-1
DISCUSSION
The diagnosis of primary melanoma of the uterine cervix is achievable due to the description of melanocytic cells in cervical epithelium9,10. The scarcity of this condition is well documented, as most of the literature consists in case reports2,11,12. The present case was diagnosed in an older patient with a deep lesion, which was challenging to diagnose, and despite undergoing surgery, chemotherapy, and radiation therapy, proved incurable.
Patients with primary melanoma are often diagnosed after 60 years of age9. Discharge or bleeding is typically the main presenting symptom; however, early lesions are frequently detected in asymptomatic patients during gynecological examination6. In the present case, the onset of bleeding prompted the patient to seek specialized care immediately, initiating her first treatment 44 days after the onset of symptoms. This duration is described in the literature with varying degrees but is often reported as relatively short6.
The initial biopsy in this case was not accurately diagnosed. Most lesions are amelanotic and thus, immunohistochemistry is necessary for confirmation of diagnosis. Expressions of protein S-100, Melan-A, and HMB-45 are often seen13-15. The former two proteins were present in this case. No cervical alterations caused by HPV (Human Papilloma Virus) were detected, and p16 (INK4), which is a surrogate marker for persistent HPV infection16, was not expressed.
The tumor was initially clinically staged as FIGO IB1 cervical cancer and later confirmed through pathological examination (pIB1). However, following immunohistochemical confirmation of melanoma, the authors inferred a grim prognosis for such an aggressive neoplasm and highlighted limited treatment options17. Radical surgery is advocated as the preferred approach, though the necessity of lymphadenectomy remains a subject of debate in the absence of metastasis evidence18.
Adjuvant chemotherapy and radiation therapy are usually administered, and neoadjuvant chemotherapy-radiation treatment may also be used3. The adjuvant treatment, however, took longer to commence due to a lengthier diagnostic process. Whether this extended period between surgical treatment and the initiation of adjuvant therapy contributed to a poor outcome cannot be conclusively stated, as cervical melanoma is known to be an aggressive neoplasm. This likely remained the primary factor influencing the unfavorable progression of the case. Dacarbazine has been extensively utilized, showing response rates of 15 to 20%; treatment regimens involving cisplatin, vinblastine, and dacarbazine/bleomycin did not yield superior results19.
More recently, the use of immune check point inhibitors appears to be a favorable option. In one study with nivolumab20, two patients with post-operative recurrence were in remission at 33 and 17 months respectively. In another study, pembrolizumab21 for high-risk stage III skin melanoma resulted in statistically significant longer recurrence-free survival compared to placebo, whereas, for aggressive cervical melanoma, poor response to the medication led to an overall survival of only six months22.
In this case, a conventional treatment regimen, supplemented with carmustine, was selected considering the aggressiveness of the disease, but unfortunately, it proved unsuccessful.
CONCLUSION
Melanoma of the uterine cervix is a rare condition that is frequently difficult to diagnose definitively. Upon confirmation of diagnosis through immunohistochemistry, a thorough search for skin and other mucosal lesions should be conducted to determine the presence of metastases. Given the rarity and poor prognosis of cervical melanoma, multi-center studies may be necessary to establish the optimal treatment approach.
ACKNOWLEDGEMENT
The authors thank the following physicians for their support in managing treatment approaches: Lícia Violeta de Souza, Iraldo Jasé dos Santos, José Geraldo Dantas bezerra, and Maria Luciene Santos.
CONTRIBUTIONS
Carlos Anselmo Lima and Marcela Sampaio Lima contributed to the study design, data collection and critical analysis of the results. Carlos Anselmo Lima, Adriana Cardoso Batista Albuquerque and Érika de Abreu Costa Brito contributed to the wording of the manuscript. All the authors revised and approved the final version for publication.
DECLARATION OF CONFLICT OF INTERESTS
There is no conflict of interests to declare.
FUNDING
None.
REFERENCES
1. Tomicic J, Wanebo HJ. Mucosal melanomas. Surg Clin North Am. 2003;83(2):237-52.
2. Asghar AH, Rizvi S, Ahmed A, et al. Primary malignant melanoma of the uterine cervix. J Cancer Allied Spec. 2016;2(1).
3. Min KJ, Kim YS, Hong JH, et al. Primary malignant melanoma of uterine cervix: a suggestion of new scheme of treatment combination. Chinese J Cancer Res. 2014;26(3):351.
4. Arık D, Öge T, Kabukçuoğlu S, et al. Amelanotic malignant melanoma of the uterine cervix diagnosed by cervical smear. Diagn Cytopathol. 2016;44(6):535-7.
5. Spencer KR, Mehnert JM. Mucosal melanoma: epidemiology, biology and treatment. Cancer Treat Res. 2016;167:295-320.
6. Pusceddu S, Bajetta E, Carcangiu ML, et al. A literature overview of primary cervical malignant melanoma: an exceedingly rare cancer. Crit Rev Oncol Hematol. 2012;81(2):185-95.
7. Conselho Nacional de Saúde (BR). Resolução n° 466, de 12 de dezembro de 2012. Aprova as diretrizes e normas regulamentadoras de pesquisas envolvendo seres humanos. Diário Oficial da União, Brasília, DF. 2013 jun 13; Seção I:59.
8. Pecorelli S. Revised FIGO staging for carcinoma of the vulva, cervix, and endometrium. Int J Gynaecol Obstet. 2009;105(2):103-4
9. Mihajlovic M, Vlajkovic S, Jovanovic P, et al. Primary mucosal melanomas: a comprehensive review. Int J Clin Exp Pathol. 2012;5(8):739-53.
10. Chang D, Tiburzio GB. Melanosis of the uterine cervix: a case report and literature review. J Bras Patol e Med Lab. 2013;49(3):222-4.
11. Mordel N, Mor-Yosef S, Ben-Baruch N, et al. Malignant melanoma of the uterine cervix: case report and review of the literature. Gynecol Oncol. 1989;32(3):375-80.
12. Deshpande AH, Munshi MM. Primary malignant melanoma of the uterine cervix: report of a case diagnosed by cervical scrape cytology and review of the literature. Diagn Cytopathol. 2001;25(2):108-11.
13. Bhargava S, Mogra N, Goyal N. Primary malignant melanoma of uterine cervix. J Obstet Gynecol India. 2014;64(S1):132-3.
14. Tsai YJ, Shueng PW, Chan SC, et al. Uterine cervical melanoma presenting with rapid progression detected by PET/CT. Acta Radiol Short Reports. 2012;1(4):16.
15. Tsai YJ, Shueng PW, Chan SC, et al. Uterine Cervical Melanocytic Tumours - a single institution experience with review of literature. Open J Obstet Gynecol. 2016;6(5):280-6.
16. Brown CA, Bogers J, Sahebali S, et al. Role of protein biomarkers in the detection of high-grade disease in cervical cancer screening programs. J Oncol 2012;1-11.
17. Yee KLC, Shukor SA, Sim WW. Primary malignant melanoma of cervix – a rare entity with limited therapeutic option. MJM Case Reports. 2022;1(1):12-16.
18. Pang Y, Yuan H, Ren A, et al. Primary malignant melanoma of the female genital tract synchronously involving the vulva and uterine cervix. Medicine (Baltimore). 2019; 98(30):e16366. doi: https://doi.org/10.1097/MD.0000000000016366.
19. Garbe C, Eigentler TK, Keilholz U, et al. Systematic review of medical treatment in melanoma: current status and future prospects. Oncologist. 2011;16(1):5-24.
20. Ankon M, Nakamura M, Kobayashi Y, et al. Primary malignant melanoma of the uterine cervix or vagina which were successfully treated with nivolumab. J Obstet Gynaecol Res. 2020;46(1):190-5.
21. Eggermont AMM, Blank CU, Mandala M, et al. Adjuvant pembrolizumab versus placebo in resected stage iii melanoma. N Engl J Med. 2018;378:1789-801.
22. Suzuki R, Endo H, Sasaki T, et al. Primary malignant melanoma of uterine cervix treated with pembrolizumab as adjuvant immunotherapy. Int Cancer Conf J. 2021;10:254-8.
Recebido em 29/9/2023
Aprovado em 11/12/2023
Scientific-Editor: Anke Bergmann. Orcid iD: https://orcid.org/0000-0002-1972-8777
Este é um artigo publicado em acesso aberto (Open Access) sob a licença Creative Commons Attribution, que permite uso, distribuição e reprodução em qualquer meio, sem restrições, desde que o trabalho original seja corretamente citado.
©2019 Revista Brasileira de Cancerologia | Instituto Nacional de Câncer | Ministério da Saúde