CASE REPORT
Atypical Breast Reconstruction Case: Report of the Use of Rectus Abdominis Myocutaneous Flap for Deformity Treatment in Major Pectoral Flap Donor Area
Caso Atípico de Reconstrucción Mamaria: Informe del Uso de Colgajo Miocutáneo del Recto Abdominal para Tratar la Deformidad en la Zona Donante del Colgajo de Pectoral Mayor
https://doi.org/10.32635/2176-9745.RBC.2024v70n2.4708
Julia Gabriela Oliveira Marchiori1; Bruno Guilherme Zampiri de Pieri2; Alfredo Benjamim Duarte da Silva3; Anne Karoline Groth4
1Hospital São Vicente. Curitiba (PR), Brasil. E-mail: juliamarchiori1@hotmail.com. Orcid iD: https://orcid.org/0000-0002-0971-6131
2-4Erasto Gaertner Hospital, Curitiba (PR), Brasil. E-mails: brunozpieri@gmail.com; alf12901@gmail.com; annegroth@gmail.com. Orcid iD: https://orcid.org/0000-0001-6496-1722; Orcid iD: https://orcid.org/0000-0001-5334-6898; Orcid iD: https://orcid.org/0000-0001-9888-3099
Corresponding author: Julia Gabriela Oliveira Marchiori. Rua Visconde do Rio Branco, 1810 – Centro. Curitiba (PR), Brasil. CEP 80420-210. E-mail: juliamarchiori1@hotmail.com
ABSTRACT
Introduction: Even with the advent of microsurgical techniques, the pedicled pectoralis major myocutaneous flap (MMF) still has considerable importance in head and neck reconstructions. However, its utilization is quite challenging especially in women. Case report: Female patient, 38 years-old sought medical attention due to a left cervical mass of progressive growth. After investigation with nuclear magnetic resonance imaging, radical cervical emptying was indicated, requiring immediate reconstruction with MMF. Subsequently, the patient returned complaining of asymmetry on the breasts and the volume of the cervical flap and a new surgical approach was performed by the plastic surgery team, where the left breast was reconstructed with a transverse rectus abdominis myocutaneous (TRAM) flap, and the MMF was thinned. Conclusion: The MMF should be used sparingly in women since resulting dysmorphisms often require surgical re-administration for reconstruction. Therefore, it is preferable to use free flaps as a first option.
Key words: Head and Neck Neoplasms/surgery; Microsurgery/methods; Myocutaneous Flap/surgery.
RESUMO
Introdução: Mesmo com o advento das técnicas microcirúrgicas, o retalho miocutâneo de peitoral maior (RMPM) ainda tem considerável importância nas reconstruções de cabeça e pescoço. No entanto, existem vários desafios ao empregá-lo, especialmente em mulheres. Relato do caso: Paciente, sexo feminino, 38 anos, procurou atendimento médico por causa de uma massa cervical esquerda de crescimento progressivo. Após investigação com ressonância nuclear magnética, foi indicado esvaziamento cervical radical, sendo necessária a reconstrução imediata com RMPM. Posteriormente, a paciente retornou com queixa de assimetria entre as mamas e do volume do retalho cervical. Assim, foi realizada nova abordagem cirúrgica pela equipe de cirurgia plástica, na qual a mama esquerda foi reconstruída com retalho miocutâneo de reto abdominal (TRAM) e o RMPM teve o seu volume reduzido. Conclusão: O RMPM deve ser usado com moderação em mulheres, pois os dismorfismos causados muitas vezes requerem correção cirúrgica. Dessa forma, é preferível utilizar retalhos microcirúrgicos como primeira opção.
Palavras-chave: Neoplasias de Cabeça e Pescoço/cirurgia; Microcirurgia/métodos; Retalho Miocutâneo/cirurgia.
RESUMEN
Introducción: Incluso con el advenimiento de las técnicas microquirúrgicas, el colgajo miocutáneo de pectoral mayor (CMPM) todavía tiene una importancia considerable en las reconstrucciones de cabeza y cuello. Sin embargo, existen varios desafíos a la hora de emplearlo, especialmente en mujeres. Informe del caso: Paciente femenina, 38 años, consultó por presentar masa cervical izquierda de crecimiento progresivo. Tras investigación con resonancia magnética nuclear se indicó disección radical de cuello, requiriendo reconstrucción inmediata con CMPM. Posteriormente, la paciente regresó quejándose de asimetría entre las mamas y el volumen del colgajo cervical. Por lo anterior, se realizó un nuevo abordaje quirúrgico por parte del equipo de cirugía plástica, en el cual se reconstruyó la mama izquierda con un colgajo miocutáneo de recto abdominal (TRAM) y se redujo el volumen del CMPM. Conclusión: El CMPM debe usarse con moderación en mujeres, ya que los dismorfismos causados a menudo requieren corrección quirúrgica. Por tanto, es preferible utilizar colgajos microquirúrgicos como primera opción.
Palabras clave: Neoplasias de Cabeza y Cuello/cirugía; Microcirugía/métodos; Colgajo Miocutáneo/cirugía.
INTRODUCTION
Head and neck repair surgery has undergone numerous advances in recent times due to the advent of microsurgical techniques. In this way, large tissue defects can be reconstructed safely, and achieve excellent aesthetic and functional results.
However, the pedicled flap still plays a key role in many centers due to its reduced cost and shorter surgical time1. Among the most important pedicled flaps in the head and neck, the pectoralis major myocutaneous flap (MMF) stands out.
Nonetheless, the use of this flap in women is challenging: the surgery often culminates in asymmetry of the breasts and the flap becomes very voluminous due to the presence of breast tissue2,3. Furthermore, another possible complication, even if rare, is the malignancy of the transplanted breast tissue.
Given this, the objective of this study was to report the case of a woman who needed a microsurgical flap to correct defects generated by an MMF reconstruction.
The study was approved by the research ethics committee of the “Pontifícia Universidade Católica do Paraná”, report number 4255241 (CAAE (submission for ethical review): 36546720.9.0000.0020), in compliance with Directive 466/20124 of the National Health Council.
CASE REPORT
A 38-year-old woman, smoker, was referred to the head and neck service of “Hospital Erasto Gaertner”, Curitiba, Paraná, Brazil. She reported a history of progressive cervical mass with four months of evolution associated with dysphagia, nausea, and night sweating, without previous comorbidities and no history of family cancer. On physical examination, a hardened mass of about 5 cm adhered to deep planes was noticed.
Magnetic resonance imaging of the region was requested for further investigation which indicated a mass in the internal jugular chain of 5.9 x 4.8 x 4.9 cm in its major axis, suggestive of malignancy. Fine-needle aspiration of the mass was performed, but the biopsy was inconclusive due to the small sample collected. In addition, a PET/CT ruled out the presence of distant metastases. Breast ultrasound or mammography was not requested preoperatively.
Approximately two months after the diagnosis, radical cervical dissection was performed and expanded to the left by the oncological surgery team. Due to the impossibility of primary closure and the need to reduce the operative time, MMF was chosen. The histological picture and immunohistochemical profile of the surgical specimens were compatible with squamous cell carcinoma. Adjuvant radiotherapy was applied because of the locally advanced disease (T3N2M0).
About one year after the end of radiotherapy, the patient did not accept the aesthetic sequelae of the MMF, due to the asymmetry of the breasts and the large volume on the cervical region, reason for which she was evaluated by the plastic surgery team of the same hospital (Figure 1).

Figure 1. Late post-operative appearance (about a year and a half after the first surgical approach). Deformity on the left breast and voluminous flap on left cervical region can be observed
Reconstruction of the left breast was proposed with a transverse rectus abdominis myocutaneous flap (TRAM), in which the lateral and medial regions of the rectus abdominis muscle were preserved (MS-2 TRAM). The chosen recipient vessels were the internal thoracic vessels. An end-to-end anastomosis was performed with simple 9-0 nylon sutures between the inferior epigastric artery and vein and the internal thoracic artery and vein. It was decided to perform primary closure of the aponeurosis and reinforcement with polypropylene mesh. The remainder of the donor area was closed using the same technique as in classic abdominoplasty. MMF was refined by incising the lower cervical scar (approximately 50% of the flap circumference), elevating the skin flap, and resecting excess subcutaneous and glandular breast tissue (Figure 2A). The resulting piece was sent to anatomopathological study, which showed normal breast tissue, without cellular atypia (Figure 2B).
The postoperative period was uneventful (Figure 3A), and she was discharged on the fourth day after surgery (Figure 3B).
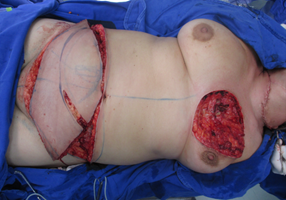

Figures 2A and 2B. Intraoperative reconstructive surgery
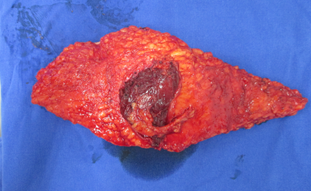
Figure 3A. MMF refinement product

Figure 3B. Appearance in the second month after surgery
DISCUSSION
First described by Ariyan2, MMF was defined as a true “workhorse” due to its good versatility for tissue repairs to the head and neck3. Its main indications are reconstructions of the middle and lower third of the face, the floor of the mouth, the neck, and the esophagus.
Its wide application can be justified by the constant anatomy, robust vascularization, technical ease, and abundant volume of soft tissues. The presence of breast tissue in women is a complicating factor since dysmorphisms frequently occur on the breast and the tissue island tends to become very bulky2. To minimize these situations, it is possible to use the pectoralis major myofascial flap, where the subcutaneous and mammary planes are not included5.
The malignancy of the transplanted breast tissue is an extremely rare complication since there are only three cases described in the literature, but it seems reasonable to be concerned about this possibility since breast cancer is frequent among women and there is an increasing number of female patients with tumors in the cervicofacial region needing reconstruction5-7. Thus, a clinical evaluation before surgery is recommended to detect history risk factors and careful examination of the breasts to find nodules. In addition, mammography and breast ultrasonography are crucial tools for early identification of this tumor, so they should be routinely requested before reconstructive surgery6-8.
In recent decades, the MMF has been gradually seen as a "rescue flap", including head and neck reconstructions, due to the diffusion of microsurgery9. So, it is used as a first option in cases of free flap failure in patients who have a contraindication of microsurgery, or in services where this technique is not available10. The main limitations of microsurgery are the high cost, prolonged surgical time, and the lack of qualified professionals to perform this technique10. However, free flaps have excellent results, with success rate close to 95%, in addition to reconstructing more complex and extensive defects11.
Had the free flap been used during the first surgery, the patient would be spared from breast and cervical deformities and she would not need to undergo a large-scale breast reconstruction surgery and refinement of the MMF. In addition, the risk of flap malignancy would not exist. In her case, anterolateral thigh or antebrachial radial flaps could have been chosen for cervical reconstruction due to the reliability, tissue correspondence, and lower morbidity of the donor area11,12.
CONCLUSION
In women, the pedicled pectoralis major myocutaneous flap should be avoided due to the significant morbidity of the donor area and the risk of transporting breast tissue to the neck, making it difficult to track and diagnose breast cancer early.
The argument of performing a faster and cheaper procedure falls apart in this case since the cost of performing the MMF was added to a second surgery: a microsurgical reconstruction for the breast and mastectomy in the cervical region. Therefore, microsurgical reconstruction should be used in these cases.
CONTRIBUTIONS
All the authors contributed to the study design, collection of information and wording of the manuscript. They approved the final version to be published.
DECLARATION OF CONFLICT OF INTERESTS
There is no conflict of interest to declare.
FUNDING SOURCES
None.
REFERENCES
1. Menezes MB, Saleh KS, Nakai MY, et al. Pectoralis major myocutaneous flap in head and neck surgery reconstructions: critical analysis. Rev Col Bras Cir. 2018;42(2):e1682
2. Ariyan S. The pectoralis major myocutaneous flap. A versatile flap for reconstruction in the head and neck. Plast Reconstr Surg. 1979;63(1):73-81
3. Mehta S, Agrawal J, Pradhan T, et al. Preservation of aesthetics of breast in pectoralis major myocutaneous flap donor site in females. J Maxillofac Oral Surg. 2016;15(2):268-71
4. Conselho Nacional de Saúde (BR). Resolução n° 466, de 12 de dezembro de 2012. Aprova as diretrizes e normas regulamentadoras de pesquisas envolvendo seres humanos. Diário Oficial da União, Brasília, DF. 2013 jun 13; Seção I:59.
5. Zbar RIS, Funk GF, McCulloch TM, et al. Pectoralis major myofascial flap: a valuable tool in contemporary head and neck reconstruction. Head Neck. 1999;19(5):412-8.
6. Maas CS, Gnepp DR, Rosenblum BN, et al. Breast cancer within a pectoralis major myocutaneous flap. Otolaryngol head neck Surg. 1988;99(6):594-6
7. Nestle-Kraemling C, Kubler N, Janni W, et al. Breast cancer in the lower jaw after reconstructive surgery with a pectoralis major myocutaneous flap (PMMC) - a case report. Eur J Med Res. 2011;16(12):553
8. Hirai E, Sarukawa S, Yamamoto K, et al. Breast cancer in a pectoralis major myocutaneous flap used for the reconstruction of the tongue cancer: a case report. J Oral Maxillofac Surg. 2017;75(7):1569.e1-7
9. Wong CH, Wei FC. Microsurgical free flap in head and neck reconstruction. Head neck. 2010;32(9):1236-45
10. Cannady SB, Hatten K, Max MK. Postoperative controversies in the menagement of free flap surgery in the head and neck. Facial Plast Surg North Am. 2016;24(3):309-14.
11. Liang J, Yu T, Wang X, et al. Free tissue flaps in head and neck reconstrution: clinical application and analysis of 93 patients of a single institution. Braz J Otorhinolaryngol. 2018;84(4):416-25.
12. Lawson BR, Moreno MA. Head and neck reconstruction with chimeric anterolateral thigh free flap. Otolaryngol head and neck Surg. 2016;154(1):59-65
Recebido em 6/5/2024
Aprovado em 5/6/2024
Scientific-editor: Anke Bergmann. Orcid iD: https://orcid.org/0000-0002-1972-8777
![]()
Este é um artigo publicado em acesso aberto (Open Access) sob a licença Creative Commons Attribution, que permite uso, distribuição e reprodução em qualquer meio, sem restrições, desde que o trabalho original seja corretamente citado.