CASE REPORT
Poorly Differentiated Large Cell Neuroendocrine Carcinoma of the Transverse Colon: Case Report
Carcinoma Neuroendócrino de Grandes Células Mal Diferenciado de Cólon Transverso: Relato de Caso
Carcinoma Neuroendocrino de Células Grandes Pobremente Diferenciado de Colon Transverso: Informe de Caso
https://doi.org/10.32635/2176-9745.RBC.2024v70n3.4725
Marianne de Lima Silva¹; Thiago Menezes Costa²; Tathiane da Silva Oliveira3; Táffines Rumenic Teodoro Machado4; Carlos Anselmo Lima5
1-4Empresa Brasileira de Serviços Hospitalares (Ebserh), Universidade Federal de Sergipe (UFS), Hospital Universitário (HU). Aracaju (SE), Brasil. E-mails: mariannelimas95@gmail.com; tmc.onco@yahoo.com.br; tathianesoliveira@hotmail.com; taffinesrumenic@gmail.com. Orcid iD: https://orcid.org/0000-0002-0685-9970; Orcid iD: https://orcid.org/0000-0003-3536-6021; Orcid iD: https://orcid.org/0009-0009-9350-4630; Orcid iD: https://orcid.org/0009-0006-0143-5366
5Ebserh/UFS/HU, Programa de Pós-Graduação em Ciências da Saúde. Aracaju (SE), Brasil. E-mail: ca.lima01@gmail.com. Orcid iD: http://orcid.org/0009-0002-1019-0584
Corresponding author: Marianne de Lima Silva. Rua Palmira Ramos Teles, 1600, bloco natura, apto. 704 – Luzia. Aracaju (SE), Brasil. CEP 49045-706. E-mail: mariannelimas95@gmail.com
ABSTRACT
Introduction: Neuroendocrine carcinomas (NECs) of the colon and rectum are extremely rare malignant subtypes of neuroendocrine tumors, with a reported incidence of 0.1% to 3.9% of all colorectal malignancies. Large cell neuroendocrine carcinomas of the colon (LCNECs) are even rarer, aggressive in nature and have a poor prognosis due to their tendency to early metastasis. Case report: Large cell neuroendocrine carcinoma in the transverse colon with liver metastasis of a 66 years- old male patient, who reported cramping abdominal pain for two months, weight loss of 12 kilos and melena during this period. Abdominal tomography showing circumferential parietal thickening with an infiltrative and stenosing appearance in the transverse colon on the right and multiple hypovascular solid hepatic nodules. Pathology of the lesion compatible with poorly differentiated carcinoma and liver metastases was metastatic adenocarcinoma. Material from the colon biopsy and liver lesions were sent for immunohistochemical studies confirming the diagnosis of high-grade neuroendocrine carcinoma. Conclusion: Early detection can offer a better prognosis for other patients and correct diagnosis is of great importance, as they are often misdiagnosed as adenocarcinoma or another malignant tumor on first imaging or histological study.
Key words: Neoplasm Metastasis; Colon, Transverse/pathology; Liver Neoplasms; Neuroendocrine Carcinoma; Abdominal pain.
RESUMO
Introdução: Os carcinomas neuroendócrinos (NEC) de cólon e reto são um subtipo maligno extremamente raro de tumores neuroendócrinos, com uma incidência relatada de 0,1% a 3,9% de todas as malignidades colorretais. Os carcinomas neuroendócrinos de grandes células do cólon (LCNEC) são ainda mais raros, com natureza agressiva e de mau prognóstico em razão da sua tendência para metástases precoces. Relato do caso: Carcinoma neuroendócrino de grandes células no cólon transverso com metástase no fígado de um paciente do sexo masculino, 66 anos, com relato de dor abdominal tipo cólica há dois meses, perda ponderal de 12 quilos e melena nesse período. Tomografia de abdome com achado de espessamento parietal circunferencial de aspecto infiltrativo e estenosante em cólon transverso à direita e múltiplos nódulos hepáticos sólidos hipovasculares. Anatomopatológico da lesão compatível com carcinoma pouco diferenciado e das metástases hepáticas de adenocarcinoma metastático. O material da biópsia do cólon e das lesões hepáticas foi encaminhado para realização de estudo imuno-histoquímico, confirmando o diagnóstico de carcinoma neuroendócrino de alto grau. Conclusão: A detecção precoce pode oferecer um melhor prognóstico a outros pacientes e o diagnóstico correto é de grande importância, uma vez que são frequentemente diagnosticados erroneamente como adenocarcinoma ou outro tumor maligno na primeira imagem ou estudo histológico.
Palavras-chave: Metástase Neoplásica; Colo Transverso/patologia; Neoplasias Hepáticas; Carcinoma Neuroendócrino; Dor abdominal.
RESUMEN
Introducción: Los carcinomas neuroendocrinos (NEC) de colon y recto son un subtipo maligno extremadamente raro de tumores neuroendocrinos, con una incidencia reportada del 0,1% al 3,9% de todas las neoplasias malignas colorrectales. Los carcinomas neuroendocrinos de colon de células grandes (LCNEC) son aún más raros, de naturaleza agresiva y de mal pronóstico debido a su tendencia a la metástasis temprana. Informe del caso: Carcinoma neuroendocrino de células grandes en colon transverso con metástasis hepática de un paciente masculino de 66 años de edad, quien refirió dolores abdominales tipo cólico de dos meses de evolución, pérdida de peso de 12 kilos y melena durante este período. Tomografía abdominal que muestra engrosamiento parietal circunferencial de aspecto infiltrativo y estenosante en colon transverso derecho y múltiples nódulos hepáticos sólidos hipovasculares. La patología de la lesión compatible con carcinoma poco diferenciado y la metástasis hepática fue adenocarcinoma metastásico. Se envió material de biopsia de colon y lesiones hepáticas para estudios inmunohistoquímicos que confirmaron el diagnóstico de carcinoma neuroendocrino de alto grado. Conclusión: La detección temprana puede ayudar a proporcionar un mejor pronóstico para futuros pacientes y el diagnóstico correcto es de gran importancia, ya que muchas veces son mal diagnosticados como adenocarcinoma u otro tumor maligno en la primera imagen o estudio histológico.
Palabras clave: Metástasis de la Neoplasia; Colon Transverso/patologia; Neoplasias Hepáticas; Carcinoma Neuroendocrino; Dolor abdominal.
Neuroendocrine tumors can develop in many different sites in the body, but are rarely found in the colon as a primary site1,2, accounting for 1% of colorectal neoplasms and 4% of neuroendocrine tumors3. Neuroendocrine carcinomas (NECs) of the colon and rectum are a rare malignant subtype of neuroendocrine tumors, with an incidence of 0.1% to 3.9% of all colorectal malignancies. These tumors are poorly differentiated, very aggressive and have a dismal prognosis, with around 70% of patients presenting metastatic disease at diagnosis and a reported average survival of between 5 and 11 months4-6.
Large cell neuroendocrine carcinomas of the colon (LCNECs) are even rarer, accounting for around 0.25% of colorectal cancers7, with a poor prognosis due to their tendency to metastasize early4,8. Of the patients with colorectal cancer, 0.6% of them were NECs, and of these, only 0.2% were large cell (LCNCEs)5,9.
Neuroendocrine tumors are a large group of neoplasms of epithelial origin with neuroendocrine differentiation and the potential to release hormones10. Their incidence has increased worldwide, presumably due to better diagnostic methods1,11. The general average age at diagnosis is 63 years9. They have a female predominance of 2.5:1, and the most prevalent primary sites are the gastrointestinal tract (62%-67%) and the lung (22%-27%)11. In the gastrointestinal tract, the most common sites are the small intestine (38%), rectum (34%), large intestine (16%), stomach (11%) and unknown sites (1%)5,11.
A rare case of large cell neuroendocrine carcinoma in the transverse colon with metastasis to the liver will be presented, with clinical and imaging characteristics similar to those of metastatic colonic adenocarcinoma, but with completely different treatment and prognosis. The study was approved by the Institutional Review Board of “Universidade Federal de Sergipe”, CAAE (submission for ethical review) number 78150123.4.0000.5546, report 6,745,843 in compliance with Directive 466/201212 of the National Health Council.
CASE REPORT
A 66-year-old white male patient, who smoked thirty cigarette packs a year and had been a daily alcoholic for forty years, reported, at his first medical appointment in November 2022, colicky abdominal pain, mostly in the left iliac fossa, for about two months, associated with weight loss of 12 kilos and episodes of melena. Colonoscopy or any other screening tests have never been performed so far. On physical examination, he presented a globose abdomen, with solid mass on the left flank and iliac fossa and hepatomegaly. Laboratory tests were unchanged. Contrast-enhanced abdominal tomography showed circumferential parietal thickening with an infiltrative and stenosing aspect in the right transverse colon, multiple solid hypovascular hepatic nodules, forming conglomerates, suggestive of secondary implants and lymph node enlargement (Figure 1).
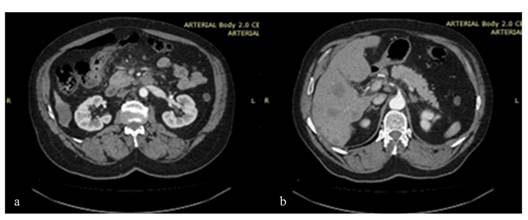
Figure 1. Abdominal CT scan showing thickening with a stenosing aspect and infiltration by the contrast medium, in the proximal segment of the transverse colon (a). Multiple randomly distributed hypovascular nodules in the liver (b)
He then underwent a colonoscopy which showed diverticular disease and a stenosing lesion of the proximal transverse colon, whose pathology was compatible with poorly differentiated carcinoma infiltrating the mucosa. Due to the risk of obstruction, he was evaluated by the surgical oncology and an exploratory laparotomy was performed in early December 2022.
Intraoperatively, an unresectable tumor was found in the hepatic angle of the colon, invading the duodenum, pancreas and retroperitoneum, and an ileocolic and gastrojejunal shunt was chosen, as well as biopsies of the liver lesions. There were no post-operative complications, but the patient had abdominal pain and inappetence after the procedure. The anatomopathological study of the liver metastases revealed metastatic adenocarcinoma. The immunohistochemical study of the colon biopsy and liver lesions showed expression of the proteins synaptophysin, chromogranin A, CDX2, SATB2, insulinoma-associated protein and cytokeratins, as well as Ki67 80%, confirming the diagnosis of high-grade neuroendocrine carcinoma (Figure 2).
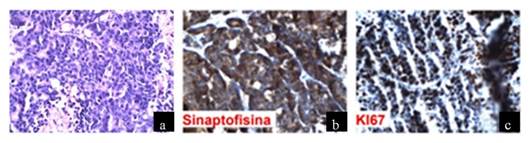 |
Figure 2. The morphological findings are of a malignant neoplasm composed of blocks of epithelioid cells of intermediate to large size (a). The immunohistochemical study reveals positivity for INSM-1, synaptophysin (b) and chromogranin A. The cell proliferation index is 80% (c)
In view of this, the clinical oncologist indicated palliative chemotherapy in December 2022 with carboplatin and etoposide; he underwent three cycles, presenting asthenia as the main adverse effect, as well as a decline in general condition. A restaging CT scan showed progression of liver and lymph node disease in February 2023. The chemotherapy was changed to second-line irinotecan. One cycle was carried out, but there was no clinical response and the patient died of liver failure on April 7, 2023.
DISCUSSION
The clinical presentation of LCNEC is similar to other colonic carcinomas, the main symptoms are abdominal pain, anemia, hematochezia, melena, constipation, tenesmus and weight loss1,2,9. The patient had marked weight loss, abdominal pain and episodes of melena. Imaging features include irregular circumferential wall thickening or polypoid mass with lymphadenopathy, very similar to those of colonic adenocarcinoma9, as well as biopsy findings, requiring immunohistochemical examination for correct diagnostic confirmation7,8.
Metastasis appears as hypervascular lesions that show moderate to intense peripheral or homogeneous enhancement during the hepatic arterial phase on multiphase computed tomography or magnetic resonance imaging. Colonic adenocarcinomas often produce hypovascular hepatic metastatic lesions9. In the present case, the lesions were hypovascular.
Neuroendocrine tumors are rare, extremely aggressive, rapidly spreading and usually metastasize in 57% of the initial presentation5,9,10. When they are found, they have probably already spread by metastasizing to various organs, the most common are in the liver, followed by bones, lungs and occasionally the central nervous system5,10.
The risk factors for the development of gastrointestinal NECs are unclear, but a family history of any type of cancer is the most significant for the development of neuroendocrine tumors in all the sites investigated (lung, pancreas and gastrointestinal tract), followed by diabetes mellitus and obesity6. Patients with a history of colorectal LCNEC are slightly more likely to describe smoking1 history.
Neuroendocrine cells are present throughout the length of the intestine, pancreas and lung, and TNEs are neoplasms with different presentations and classifications, depending on their location, differentiation and stage2,4. The 2018 World Health Organization (WHO) classification divides them according to anatomical location (gastrointestinal tract (GIT), pancreas and lung); family (TNEs or NECs); and grade. In the GIT, the current terminology for TNEs is grade 1 (G1), grade 2 (G2) and grade 3 (G3), while NECs are divided into small cell neuroendocrine carcinoma and large cell neuroendocrine carcinoma11.
The aggressiveness of neuroendocrine tumors depends on several factors, as degree of differentiation, tumor size, hormone levels, chromogranin A level, number of mitoses and Ki-67 index13. As Ki-67 is related to cell replication and not DNA repair, it is an excellent marker for tumor growth. In the case reported, 80% of the tumor cell nuclei were positive for Ki-67, proving its highly aggressive nature with rapid liver metastasis4. G3 tumors, for example, have a mitotic rate of >20 per 10 HPF and a Ki-67 index of >20%6.
They usually express one or more neuroendocrine immunohistochemical markers (synaptophysin, chromogranin, neural cell adhesion molecule CD56 and neurospecific enolase)6. Serum chromogranin A can be elevated in 80% of all gastrointestinal NECs and correlates with tumor burden. Synaptophysin is diffusely positive in almost all NECs8. The nuclear expression of CDX2 found in most carcinoma cells points to the colon as the primary origin of the lesion, making it a reliable marker for cancers originating in the intestine14. In this case, chromogranin A, synaptophysin and CDX2 were expressed.
Currently, there are no standardized treatment guidelines for colorectal LCNECs8, although chemotherapy is a fundamental pillar in the treatment of patients with advanced disease15. The benefit of chemotherapy and radiotherapy, as used for classic colorectal adenocarcinomas, is not defined2. The first line of treatment for large cell neuroendocrine carcinomas has been surgery to resect the tumor, to relieve obstruction and improve survival, but a poor prognosis has been observed in most of these patients due to late diagnosis15.
Patients with advanced disease may benefit from surgery to treat tumor complications such as obstruction, bleeding and perforation, similar to this case 2,8. Platinum-based chemotherapy as an adjuvant therapeutic strategy to surgery is often used, as cisplatin/etoposide or cisplatin/irinotecan5,6,8, and the response rate is 42% for NECs which is relatively lower than 67% for small cell lung cancer15. Data is very limited on second-line agents and other effective options should be investigated5. No information was found in the literature on neoadjuvant therapy in NECs of the colon7.
CONCLUSION
There is a scarcity of articles describing large LCNECs in the literature. Therefore, more studies are needed to establish the genetics of these rare tumors and define the ideal local and systemic therapies, particularly adjuvant chemotherapy regimens. Early detection can offer a better prognosis for other patients and correct diagnosis is of great importance, as they are often misdiagnosed as adenocarcinoma or another malignant tumor on first imaging or histological study.
CONTRIBUTIONS
All the authors have substantially contributed to the study design, acquisition, analysis and interpretation of the data, wording, and critical review. They approved the final version for publication.
DECLARATION OF CONFLICT OF INTERESTS
There is no conflict of interest to declare.
FUNDING SOURCES
None.
REFERENCES
1. Corbett V, Arnold S, Anthony L, et al. Management of large cell neuroendocrine carcinoma. Front Oncol. 2021;11(653162):1-20. doi: https://doi.org/10.3389/fonc.2021.653162
2. Alloucha A, Moussa MK, Dirany A, et al. Large cell neuroendocrine carcinoma of the colon with brain metastasis: a case report. Int J Surg Case Rep. 2020;76:421-4. doi: https://doi.org/10.1016%2Fj.ijscr.2020.10.015
3. Tejero-Pintor FJ, Sarmentero-Prieto JC, Bailón-Cuadrado M, et al. Doble metástasis hepática de doble neoplasia de colon: adenocarcinoma y tumor neuroendocrino. Gastroenterol Hepatol. 2019;42:624-5. doi: https://doi.org/10.1016/j.gastrohep.2019.05.004
4. Pascarella MR, McCloskey D, Jenab-Wolcott J, et al. Large cell neuroendocrine carcinoma of the colon: a rare and aggressive tumor. J Gastrointest Oncol. 2011;2:250-3. doi: https://doi.org/10.3978/j.issn.2078-6891.2011.026
5. Felux K, McCarty B, Turner D, et al. (January 05, 2022) Poorly differentiated large cell neuroendocrine carcinoma of the colon: a case report. Cureus.14(1):e20949. doi: https://doi.org/10.7759/cureus.20949
6. Stoner P, Ghaffaripour T, Cohen D. Aggressive large-cell neuroendocrine carcinoma of the sigmoid colon in a patient with ulcerative colitis. BMJ Case Rep. 2017;2017:bcr2017220093. doi: https://doi.org/10.1136/bcr-2017-220093
7. Goksoy B, Tosun Y, Gunay MO. Multifocal diffuse large cell neuroendocrine carcinoma of the colon. J Clin Transl Res. 2022;8(4):272-5.
8. Khanna V, Reddy T, Nagar T, et al. Metastatic large cell neuroendocrine carcinoma of the colon: a case report. Cureus. 14(6):e26075. doi: https://doi.org/10.7759/cureus.26075
9. Cha JW, Yang M, Mo A. Large cell neuroendocrine carcinoma in the unusual location of the descending colon. Radiol Case Rep. 2020;15(10):1841-4. doi: https://doi.org/10.1016/j.radcr.2020.07.045
10. Bloom JR, Brickman A, Yang FJ, et al. Neuroendocrine carcinoma of the colon presenting as acute meningitis. BMC Neurol. 2019;19(76):1-4. doi: https://doi.org/10.1186/s12883-019-1310-x
11. Parra-Medina R, Moreno-Lucero P, Jimenez-Moreno J, et al. Neuroendocrine neoplasms of gastrointestinal tract and secondary primary synchronous tumors: a systematic review of case reports. casualty or causality? PLoS One. 2019;14(5):1-16. https://doi.org/10.1371/journal.pone.0216647
12. Conselho Nacional de Saúde (BR). Resolução n° 466, de 12 de dezembro de 2012. Aprova as diretrizes e normas regulamentadoras de pesquisas envolvendo seres humanos. Diário Oficial da União, Brasília, DF. 2013 jun 13; Seção I:59.
13. Lancellotti F, Solinas L, Telesco D, et al. A rare case of metachronous neuroendocrine tumor after a colorectal adenocarcinoma: qualitative critical review of synchronous and metachronous gastrointestinal NET. Clin J Gastroenterol. 2021;14:115-22. doi: https://doi.org/10.1007/s12328-020-01255-9.
14. Woischke C, Jung P, Jung A, et al. Mixed large cell neuroendocrine carcinoma and squamous cell carcinoma of the colon: detailed molecular characterisation of two cases indicates a distinct colorectal cancer Entity. J Pathol Clin Res. 2021;7:75-85. doi: https://doi.org/10.1002/cjp2.183
15. Yoshida T, Kamimura K, Hosaka K, et al. Colorectal neuroendocrine carcinoma: a case report and review of the literature. World J Clin Cases. 2019;7(14):1865-75. doi: https://doi.org/10.12998/wjcc.v7.i14.1865
Recebido em 24/5/2024
Aprovado em 5/8/2024
Scientific-editor: Anke Bergmann. Orcid iD: https://orcid.org/0000-0002-1972-8777
![]()
Este é um artigo publicado em acesso aberto (Open Access) sob a licença Creative Commons Attribution, que permite uso, distribuição e reprodução em qualquer meio, sem restrições, desde que o trabalho original seja corretamente citado.