CASE REPORT
Buccomaxillofacial Prosthesis as a Rehabilitative Alternative in Buconasal Communication: Case Report
Prótese Bucomaxilofacial como Alternativa Reabilitadora na Comunicação Buconasal: Relato de Caso
Prótesis Bucomaxilofacial como Alternativa Rehabilitadora en la Comunicación Buconasal: Informe de Caso
https://doi.org/10.32635/2176-9745.RBC.2025v71n3.5036
Sonia Groisman1; Débora Dummer Meira2; Matheus Correia Casotti3; Florence Mitsue Sekito4; Bárbara Castro da Silva Dias5; Ingrid Barros da Costa Damasceno6; Raquel Richelieu Lima de Andrade7; Lorena Souza Castro Altoé8; Elizeu Fagundes de Carvalho9; Iúri Drumond Louro10; Carlos Antônio Freire Sampaio11
1,9Universidade do Estado do Rio de Janeiro (Uerj), Instituto de Biologia Roberto Alcântara Gomes (IBRAG). Rio de Janeiro (RJ), Brasil. E-mails: soniagroisman@gmail.com; elizeufc@hotmail.com. Orcid iD: https://orcid.org/0000-0003-1153-3841; Orcid iD: https://orcid.org/0000-0003-4620-7253
2,3,8,10Universidade Federal do Espírito Santo (Ufes), Centro de Ciências Humanas e Naturais (CCHN), Departamento de Ciências Biológicas (DCBIO), Núcleo de Genética Humana e Molecular. Vitória (ES), Brasil. E-mails: debora.dummer.meira@gmail.com; matheus.c.casotti@gmail.com; lorenascast@gmail.com; iurilouro@yahoo.com. Orcid iD: https://orcid.org/0000-0002-6092-2459; Orcid iD: https://orcid.org/0000-0002-9191-8858; Orcid iD: https://orcid.org/0000-0001-6118-485X; Orcid iD: https://orcid.org/0000-0001-5160-9615
4-7,11Uerj, Faculdade de Odontologia, Departamento de Prótese. Rio de Janeiro (RJ), Brasil. E-mails: fmsekito@gmail.com; barbarasilva.uerj@gmail.com; ingridfouerj@gmail.com; raquel.pontes@hupe.uerj.br; cafsampaio68@gmail.com. Orcid iD: https://orcid.org/0000-0003-3625-8735; Orcid iD: https://orcid.org/0009-0006-3789-517X; Orcid iD: https://orcid.org/0000-0002-3899-9951; Orcid iD: https://orcid.org/0009-0002-7139-5639; Orcid iD: https://orcid.org/0009-0008-8306-8444
Corresponding author: Débora Dummer Meira. UFES, CCHN, DCBIO. Avenida Fernando Ferrari, 514 – Prédio Ciências Biológicas, Bloco A, Sala 106. Vitória (ES), Brasil. CEP 29075-910. E-mails: debora.dummer.meira@gmail.com; debora.meira@ufes.br
ABSTRACT
Introduction: Mucormycosis, a rare and aggressive fungal infection, presents a significant clinical challenge, requiring early diagnosis and effective treatment. The importance of an integrated approach to orofacial rehabilitation emphasizes the harmonious correlation between dental elements and facial structures, crucial for oral aesthetics and function. Case report: A patient with mucormycosis (zygomycosis) who suffered from oral-nasal communication after maxillectomy, highlighted the use of a maxillofacial prosthesis as an efficient non-surgical solution. The treatment included the creation of a new obturator prosthesis, using careful manufacturing techniques to adjust the weight and maximize comfort and functionality for the patient. Conclusion: Rehabilitation with oral and maxillofacial prostheses represents a viable, less invasive and cost-effective alternative, promoting the restoration of patients' aesthetics, function and social image and avoiding complex grafts. This approach benefits public health by reducing the psychosocial stress of more invasive treatments and promoting collaborative, multidisciplinary care that values diversity of concepts to reach best clinical outcomes.
Key words: Mucormycosis; Maxillofacial Injuries; Prostheses and Implants; Rehabilitation; Dental Care.
RESUMO
Introdução: A mucormicose, infecção fúngica rara e agressiva, apresenta um desafio clínico significativo, necessitando de diagnóstico precoce e tratamento eficaz. A importância de uma abordagem integrada da reabilitação orofacial, enfatizando a correlação harmoniosa entre os elementos dentários e as estruturas faciais, cruciais para a estética e função oral. Relato do caso: Paciente com infecção mucormicose (zigomicose) que, após maxilectomia, sofreu com comunicação oronasal, destacando-se o uso de prótese maxilofacial como solução não cirúrgica eficiente. O tratamento incluiu a criação de uma nova prótese obturadora, utilizando cuidadosas técnicas de fabricação para ajustar o peso e maximizar o conforto e funcionalidade do paciente. Conclusão: A reabilitação com próteses bucomaxilofaciais representa uma alternativa viável, menos invasiva e de baixo custo, promovendo a restauração da estética, função e imagem social dos pacientes sem a necessidade de enxertos complexos. Essa abordagem beneficia a saúde pública ao reduzir o estresse psicossocial de tratamentos mais invasivos e promover cuidados colaborativos e multidisciplinares que valorizam a diversidade de ideias para obter os melhores resultados clínicos.
Palavras-chave: Mucormicose; Traumatismos Maxilofaciais; Próteses e Implantes; Reabilitação; Assistência Odontológica.
RESUMEN
Introducción: La mucormicosis, una infección fúngica rara y agresiva, presenta un desafío clínico importante que requiere un diagnóstico temprano y un tratamiento eficaz. Es importante un enfoque integrado para la rehabilitación orofacial, enfatizando la correlación armoniosa entre los elementos dentales y las estructuras faciales, cruciales para la estética y la función bucal. Informe del caso: Paciente con infección por mucormicosis (zigomicosis), quien luego de maxilectomía sufrió con la comunicación oro-nasal, destacando el uso de prótesis maxilofacial como solución no quirúrgica eficiente. El tratamiento incluyó la creación de una nueva prótesis obturadora, utilizando cuidadosas técnicas de fabricación para ajustar el peso y maximizar la comodidad y funcionalidad para el paciente. Conclusión: La rehabilitación con prótesis orales y maxilofaciales representa una alternativa viable, menos invasiva y de bajo costo, promoviendo la restauración de la estética, función e imagen social de los pacientes sin necesidad de injertos complejos. Este enfoque beneficia a la salud pública al reducir el estrés psicosocial de tratamientos más invasivos y promover una atención colaborativa y multidisciplinaria que valore la diversidad de ideas para obtener los mejores resultados clínicos.
Palabras clave: Mucormicose; Traumatismos Maxilofaciais; Próteses e Implantes; Reabilitação; Assistência Odontológica.
INTRODUCTION
The smile provides a correlation of harmony among the proportions, positioning, shape and colors of the dental units and the analysis of facial structures1. Carrying out dental planning through the integration of different areas is crucial to diagnose, prognose, plan and properly execute oral rehabilitation procedures1. Factors that affect the life of an individual with poor oral health are self-perception and how they are perceived by others affecting the judgement of attractiveness and personality in addition to psychological and intellectual qualities2,3.
For patients with facial and dental deformities, they result in functional and social problems, as eating, chewing and speaking, changes in behavior, difficulty to access the job market, dissatisfaction and rejection of physical appearance4,5. Thus, orofacial rehabilitation is a public health issue, requiring rehabilitative treatment capable of counteracting social inequality6.
Among the problems of significant clinical challenges, mucormycosis, also known as zygomycosis, is a rare and potentially fatal fungal infection caused by fungi of the phylum zygomycota. The epidemiology of mucormycosis shows that, although continuing to be a relative rare mycosis, its incidence is increasingly concerning in the whole world, due to the growth of immunocompromised individuals7 (diabetic, transplanted, oncohematological, users of corticoids and, more recently, COVID-19 infected); the last, an emerging threat with clinical-epidemiologic impacts, requiring continuous surveillance, fast diagnosis and aggressive therapy to reduce mortality and sequelae.
Studies highlight that, in addition to the immunosuppressive impact inherent to oncological treatments, with the use of chemotherapy, corticosteroids and other immunomodulatory agents, the characteristics of the onco-hematological pathology itself, as acute myeloid leukemia and lymphoproliferative disorders, play a fundamental role in the predisposition to infection7-9. It is characterized by rapid dissemination of the fungus in the affected tissues, resulting in invasive fungal vasculitis. Early diagnosis of mucormycosis is challenging, as symptoms may initially mimic other fungal or bacterial infections. Effective treatment involves a combination of surgical approaches to remove infected tissue and aggressive antifungal therapy10,11.
Mucormycosis can manifest, primarily affecting the paranasal sinuses and lungs. In more severe cases, it can extend to the oral and facial cavities, leading to significant necrosis of the affected tissues, provoking intense pain and skin discoloration. The underlying mechanism involves the invasion of blood vessels by these fungi, which leads to ischemia and subsequent cell death. When the infection spreads to the orofacial region, it can result in considerable loss of tissue, including the gums, palate, and loss of bone structures further to aesthetic and functional deformities, causing difficulties in chewing and speaking12-14.
In view of the incidence of mucormycosis, a case report of a patient whose management consisted in a maxillofacial prosthesis and favorable clinical outcome, reflecting a non-surgical and beneficial treatment will be presented.
The Informed Consent Form (ICF) was signed by the patient's legal guardian, agreeing with voluntary participation in the study, which was approved by the Ethics Committee of “Universdade do Estado do Rio de Janeiro”(Uerj), report number 5.141.274, CAAE (submission for ethical review) 30641020.7.0000.5259, in compliance with Directive 466/201215 of the National Health Council.
CASE REPORT
Male patient, melanoderma, 52 years old, controlled diabetes, with a previous history of glaucoma which caused total loss of vision, was diagnosed in 2009 with a fungal infection process caused by mucormycosis, which is a rare but highly invasive infection caused by fungi of the order Mucorales, which caused necrosis of the palatal tissue. He was submitted to maxillectomy which caused buconasal communication complications as surgical sequela. In 2022, the patient was seen at the Oral and Maxillofacial Rehabilitation Clinic of Universidade do Estado do Rio de Janeiro complaining of prosthetic maladjustment. The treatment plan consisted in the creation of a new removable partial obturator prosthesis; anatomical molding was performed using irreversible hydrocolloid type II and S-5 and I-5 type Vernes trays to obtain the study model.
The plaster (irreversible hydrocolloid) was mixed with spatula and water on a mixing bowl according to the manufacturer’s recommendations and poured into the mold with alginate. The mold was inserted into the mouth for 3 to 5 minutes for the alginate to set, (depending on the brand), removed and placed on a vibrating table to reduce or remove air bubbles. As soon as the plaster dried, it was removed from the mold, discarding the alginate, which resulted in the plaster model to produce the prosthesis.
Constructing a palatal orofacial prosthesis involves several critical steps, as it is designed to restore function (speech, swallowing, and mastication) and aesthetics in patients with congenital or acquired defects, as cleft palate, maxillectomy, or other craniofacial anomalies. Below is a step-by-step guide for fabricating a palatal obturator or orofacial prosthesis: (i) create occlusal indexes in a pillar (ceiling pillar) structure, using the palatal plane and Winner circumferential clips, with the pillar dental model base for occlusal study; palatal plane reference (an anatomical guide or digital scan of the maxilla) Winner circumferential clips (for securing materials in place); (ii) establish the palatal plane reference as a stable reference to determine occlusal relationships. Anatomical landmarks were utilized for accurate alignment . The Winner circumferential clips were placed to secure the palatal reference and hold the material in place to avoid movement.
For prosthesis design and framework construction it is necessary to convert the wax model into heat-cured acrylic resin through a conventional technique, using silicone prostheses, with addition of pigments for better esthetics. At this phase, the prosthesis was tested in the patient for adjustments and polishing to ensure smooth surfaces to avoid irritation, promote stability without excessive pressure on soft tissues, and guide the patient to adapt to the prosthesis and oral hygiene.
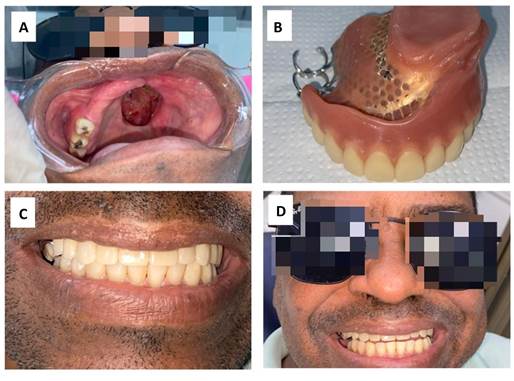
During the preparation of the prosthesis in the mouth, in the curative stage, supragingival periodontal scaling and replacement of composite resin restorations were carried out, and in the prosthetic stage, occlusal niches were prepared in pillar teeth with the palatal plate and twinned circumferential clasp as the major connector. Figure 1 shows the phases of the process.
Figure 1. Insertion of the prosthesis and rehabilitation
Captions: A = patient without the prosthesis; B = final molding and completed prosthesis; C and D = upper obturator prosthesis implanted.
DISCUSSION
The interplay between oral health and overall quality of life is well established, highlighting the importance of comprehensive dental care to promote social and psychological well-being. In this case report, the application of maxillofacial prosthetics in the management of a patient with mucormycosis highlights the profound impact of dental rehabilitation in restoring patient’s function and confidence11.
Furthermore, underlying hematologic conditions, notably acute myeloid leukemia and lymphoproliferative disorders, further aggravate the vulnerability of these patients, intensifying the risks associated with invasive fungal infections8,9. The association between mucormycosis and diabetes, particularly diabetic ketoacidosis, is well recognized, although the contribution of inadequate glycemic control to the risk in patients with other medical comorbidities is not yet clearly defined. Previous reports describe the occurrence of overt diabetes in up to 23% of immunocompromised patients with mucormycosis15. Globally, diabetes mellitus is the main underlying disease, especially in low-and middle-income countries, whereas in developed countries, hematologic malignancies and transplantation predominate16. Mucormycosis presents a multifaceted challenge in clinical practice, primarily due to its rapid progression and the complexities involved in its diagnosis and treatment11.
The epidemiology of mucormycosis has evolved with the introduction of new immunomodulatory agents used in the treatment of cancer and autoimmune diseases. Studies indicate that the most relevant conditions that predispose the development of mucormycosis include diabetes mellitus (with or without ketoacidosis), hematologic malignancies, other neoplasms, transplantation, prolonged neutropenia, use of corticosteroids, trauma, iron overload, illicit use of intravenous drugs, neonatal prematurity and malnutrition. In addition, immunocompetent patients can also be affected when the fungal spores are inoculated directly into the skin due to trauma or burns7,16. In children treated for acute lymphoblastic leukemia, the use of chemotherapy, high doses of corticosteroids or critical illness and overt hyperglycemia, constitute independent risk factors for infectious complications and worse prognosis7. Even in the absence of acidosis, elevated serum glucose levels may increase the incidence or severity of mucormycosis by inhibiting chemotactic responses to hyphae, endothelial invasion, and host cell damage.
The patient’s journey, beginning with severe necrosis of the palatal tissue and culminating in maxillectomy, reflects the harsh realities faced by individuals with invasive fungal infections. The subsequent creation of a removable partial denture represents a significant step toward restoring the patient’s oral function and mitigating the psychological distress associated with the disfigurement.
This commitment to ethical practice further enhances the credibility of the reported case and serves as a model for subsequent studies in the field. From a technical perspective, the detailed description of the prosthesis fabrication process illustrates the meticulous planning and execution required to achieve optimal results5. The choice of materials and techniques, as the use of irreversible hydrocolloid for impression making and the design of a lightweight prosthesis, demonstrates the importance of individualized treatment strategies to meet each patient’s unique challenges. The incorporation of features such as occlusal niches and circumferential clasps not only contributes to the stability of the prosthesis but also reflects a thorough understanding of biomechanics in oral rehabilitation.
CONCLUSION
A non-surgical rehabilitation option using oral and maxillofacial prosthesis provides a tailored satisfactory and less aggressive biopsychosocial rehabilitation approach to the patient, consisting in a cost-effective valuable clinical strategy and favorable outcome.
Thus, it highlights an important approach for direct application to public health, reestablishing aesthetics, function, harmonic appearance, social image, speech, feeding and swallowing capacity, being the alternative to the use of bone tissue, collagen or dermis grafts, which, in certain situations, make the use of intraoral prostheses unfeasible by hindering the formation of adequate support tissue.
Furthermore, it diminishes the possibility of further psychosocial stress associated with more surgeries and makes it difficult to monitor the operated area in relation to possible recurrences. Finally, such techniques and methodologies are extremely valuable for connecting basic and clinical research multidisciplinary groups, valuing the diversity of ideas and opinions for the best outcome for the patient in a translational way.
CONTRIBUTIONS
All the authors contributed substantially to the study design, acquisition, analysis and interpretation of the data as well as writing and critical review. They approved the final version to be published.
DECLARATION OF CONFLICT OF INTERESTS
There is no conflict of interests to declare.
FUNDING SOURCES
None.
REFERENCES
1. Vieira AC, Oliveira MCS, Andrade ACV, et al. Abordagem interdisciplinar na reabilitação estética do sorriso. Rev Odontol Araçatuba [Internet]. 2018[Acesso 2025 fev 26];39(2)54-9. Disponível em: https://revaracatuba.odo.br/revista/2018/09/TRABALHO8.pdf
2. Queiroz MF, Verli FD, Marinho SA, et al. Dor, ansiedade e qualidade de vida relacionada à saúde bucal de pacientes atendidos no serviço de urgência odontológica. Ciênc Saúde Colet. 2019;24(4):1277-86. doi: https://doi.org/10.1590/1413-81232018244.33802016
3. Närhi L, Mattila M, Tolvanen M, et al. The associations of dental aesthetics, oral health-related quality of life and satisfaction with aesthetics in an adult population. Eur J Orthod. 2023;45(3):287-94. doi: https://doi.org/10.1093/ejo/cjac075
4. Corrêa HW, Bitencourt FV, Nogueira AV, et al. Saúde bucal em usuários da atenção primária: análise qualitativa da autopercepção relacionada ao uso e necessidade de prótese dentária. Physis. 2016;26(2):503-24. doi: https://doi.org/10.1590/S0103-73312016000200009
5. Cruz JHA, Silva RLB, Andrade Júnior FP, et al. A importância da anatomia e escultura dental para prática de procedimentos clínicos odontológicos. RSC online [Internet]. 2018[Acesso 2025 fev 26];7(1):76-85. Disponível em: https://rsc.revistas.ufcg.edu.br/index.php/rsc/article/view/82/76
6. Colussi CF, Patel FS. Uso e necessidade de prótese dentária no brasil: avanços, perspectivas e desafios. Sau & Transf Soc [Internet]. 2016[Acesso 2025 fev 26];7(1):41-8. Disponível em: https://incubadora.periodicos.ufsc.br/index.php/saudeetransformacao/article/view/3707
7. Marón GA, Inagaki K, Rodriguez A, et al. Mucormycosis in children with cancer and hematopoietic cell transplant-A single center cohort study. PLoS One. 2024;19(2):e0297590. doi: https://doi.org/10.1371/journal.pone.0297590
8. Loeffen YGT, Scharloo F, Goemans BF, et al. Mucormycosis in children with hematologic malignancies: a case series and review of the literature. Pediatr Infect Dis J. 2022;41(9):e369-76. doi: https://doi.org/10.1097/inf.0000000000003608
9. Pagano L, Dragonetti G, Carolis E, et al. Developments in identifying and managing mucormycosis in hematologic cancer patients. Expert Rev Hematol. 2020;13(8):895-905. doi: https://doi.org/10.1080/17474086.2020.1796624
10. Curutchet D. Zigomicosis. Rev argent dermatol [Internet]. 2010[Acesso 2025 fev 26];91(2):39-50. Disponível em: https://www.scielo.org.ar/scielo.php?script=sci_arttext&pid=S1851-300X2010000200004&lng=es&nrm=iso&tlng=es
11. León GA, Herazo JG. Zigomicosis. Infectio. 2010;14:181-92. doi: https://doi.org/10.1016/S0123-9392(10)70135-1
12. Kirkpatrick WR, Fothergill AW. Zygomycosis: a review of the literature. Clin Microbiol Rev. 2015;28(3):557-77. doi: https://doi.org/10.1128/CMR.00001-15
13. Rodriguez JA, Kauffman CA. Mucormycosis: a review. Curr Infect Dis Rep. 2016;18(11):1-8. doi: https://doi.org/10.1007/s11908-016-0560-0
14. Bitar DJ, Lortholary O. Mucormycosis: an overview. Clin Microbiol Infect. 2014;20(1):1-10. doi: https://doi.org/10.1111/1469-0691.12400
15. Conselho Nacional de Saúde (BR). Resolução n° 466, de 12 de dezembro de 2012. Aprova as diretrizes e normas regulamentadoras de pesquisas envolvendo seres humanos. Diário Oficial da União, Brasília, DF. 2013 jun 13; Seção I:59.
16. Skiada A, Pavleas I, Drogari-Apiranthitou M. epidemiology and diagnosis of mucormycosis: an update. J Fungi (Basel) 2020;6(4):265. doi: https://doi.org/10.3390/jof6040265
Recebido em 24/12/2024
Aprovado em 25/3/2025
Associate-editor: Daniel Cohen Goldemberg. Orcid iD: https://orcid.org/0000-0002-0089-1910
Scientific-editor: Anke Bergmann. Orcid iD: https://orcid.org/0000-0002-1972-8777
![]()
Este é um artigo publicado em acesso aberto (Open Access) sob a licença Creative Commons Attribution, que permite uso, distribuição e reprodução em qualquer meio, sem restrições, desde que o trabalho original seja corretamente citado.