CASE REPORT
Pancreatic Adenocarcinoma in a Patient with IgG4-Related Autoimmune Pancreatitis: Diagnostic Challenge
Adenocarcinoma de Pâncreas em Paciente com Pancreatite Autoimune Relacionada ao IgG4: Desafio Diagnóstico
Adenocarcinoma de Páncreas en Paciente con Pancreatitis Autoinmune Relacionada con IgG4: Desafío Diagnóstico
Letícia Vieira dos Santos Ribeiro1; Vítor Paulino dos Santos2; Gilberto Kremer3; Flávia Cristina de Novaes Gerber4; Leandro Marins5; Fabiana Barroso Thomaz6; Leonardo de Lucca Schiavon7; Janaína Luz Narciso-Schiavon8
1,2Universidade Federal de Santa Catarina (UFSC), Curso de Graduação em Medicina. Florianópolis (SC), Brasil. E-mails: leticiavieirast@gmail.com; vitorpaulino.ufsc@outlook.com. Orcid iD: https://orcid.org/0009-0001-5934-8488; Orcid iD: https://orcid.org/0009-0008-6335-796X
3UFSC, Hospital Universitário Polydoro Ernani de São Thiago, Divisão do Aparelho Digestivo. Florianópolis (SC), Brasil. E-mail: gilbertokremer@yahoo.com. Orcid iD: https://orcid.org/0009-0001-3330-1403
4,5UFSC, Hospital Universitário Polydoro Ernani de São Thiago, Serviço de Anatomia Patológica. Florianópolis (SC), Brasil. E-mails: flaviacngerber@gmail.com; dr.leandromarins@gmail.com. Orcid iD: https://orcid.org/0009-0002-2184-9831; Orcid iD: https://orcid.org/0009-0009-6441-0758
6UFSC, Hospital Universitário Polydoro Ernani de São Thiago, Serviço de Radiologia. Florianópolis (SC), Brasil. E-mail: fabiana.radio@gmail.com. Orcid iD: https://orcid.org/0000-0003-4020-086X
7,8UFSC, Departamento de Clínica Médica. Florianópolis (SC), Brasil. E-mails: leo-jf@uol.com.br; janaina.narciso@uol.com.br. Orcid iD: https://orcid.org/0000-0003-4340-6820; Orcid iD: https://orcid.org/0000-0002-6228-4120
Corresponding author: Janaína Luz Narciso-Schiavon. Rua Maria Flora Pausewang, SN – Hospital Universitário, 3º andar – Trindade. Florianópolis (SC), Brasil. CEP 88036-800. E-mail: janaina.narciso@uol.com.br
ABSTRACT
Introduction: IgG4-related autoimmune pancreatitis (AIP) type 1 is a fibroinflammatory condition. An atypical case of pancreatic adenocarcinoma arising in a patient with IgG4-related AIP, which progressed despite corticosteroid therapy, raising the hypothesis of a missed malignancy at initial presentation or tumor development in the setting of chronic inflammation is reported. Case report: A 46-year-old male presented with abdominal pain, fever, and jaundice. Imaging revealed a pancreatic head mass with calcifications, pancreatic tail atrophy, and peripancreatic lymphadenopathy, raising suspicion of malignancy. During hospitalization for diagnostic workup, the patient developed cholangitis. Magnetic resonance cholangiopancreatography revealed a common bile duct stricture, managed with endoscopic retrograde cholangiopancreatography and biliary stent placement. An endoscopic ultrasound-guided biopsies were non-diagnostic. An exploratory laparotomy with open biopsy confirmed IgG4-related AIP. Despite corticosteroid therapy, the patient showed clinical deterioration with worsening abdominal pain, progressive biliary strictures, and significant weight loss. During follow-up, biliary stent exchanges became increasingly difficult due to stricture progression. Another endoscopic ultrasound-guided biopsy ultimately confirmed pancreatic adenocarcinoma. The patient was referred for palliative chemotherapy. Conclusion: The diagnosis of IgG4-related pancreatitis must be carefully established, and lack of treatment response warrants diagnostic reevaluation, as in this case, where it ultimately represented pancreatic malignancy.
Key words: Autoimmune Pancreatitis; Adrenal Cortex Hormones/therapeutic use; Pancreatic Neoplasms.
RESUMO
Introdução: A pancreatite autoimune (PAI) tipo 1, associada à IgG4, é uma condição fibroinflamatória. Relata-se um caso atípico de adenocarcinoma de pâncreas em paciente com diagnóstico prévio de PAI relacionada ao IgG4, que evoluiu apesar da terapia com corticosteroides, levantando a hipótese de uma neoplasia não diagnosticada na apresentação inicial ou do desenvolvimento tumoral no contexto de inflamação crônica. Relato do caso: Homem, 46 anos, apresentou-se com dor abdominal, febre e icterícia. A tomografia revelou uma massa na cabeça do pâncreas, associada a calcificações, atrofia do pâncreas distal e linfadenopatia peripancreática, sugerindo malignidade. Durante a internação para investigação diagnóstica, o paciente evoluiu com colangite. A colangiorressonância magnética demonstrou estenose do ducto biliar comum, tratada por meio de colangiopancreatografia retrógrada endoscópica com colocação de prótese biliar. A biópsia guiada por ultrassom endoscópico foi não diagnóstica. Uma laparotomia exploradora com biópsia aberta confirmou o diagnóstico de PAI relacionada ao IgG4. Apesar do uso de corticosteroides, o paciente apresentou piora clínica, com dor abdominal crescente, progressão das estenoses biliares e perda de peso significativa. Durante o seguimento, as trocas de prótese biliar tornaram-se progressivamente mais difíceis em razão da acentuação das estenoses. Uma nova biópsia guiada por ultrassom endoscópico confirmou, por fim, o diagnóstico de adenocarcinoma de pâncreas. O paciente foi encaminhado para quimioterapia paliativa. Conclusão: O diagnóstico de PAI relacionado ao IgG4 deve ser estabelecido criteriosamente, e a ausência de resposta ao tratamento deve motivar reavaliação diagnóstica, como neste caso em que o quadro representava, na verdade, uma neoplasia pancreática subjacente.
Palavras-chave: Pancreatite Autoimune; Corticosteroides/uso terapêutico; Neoplasias Pancreáticas.
RESUMEN
Introducción: La pancreatitis autoinmune (PAI) tipo 1 asociada a la IgG4 es una condición fibroinflamatória. Se presenta un caso atípico de adenocarcinoma de páncreas en un paciente con diagnóstico previo de PAI relacionada con IgG4, que evolucionó a pesar del tratamiento con corticosteroides, lo que plantea la hipótesis de una neoplasia no diagnosticada en la presentación inicial o del desarrollo tumoral en el contexto de inflamación crónica. Informe del caso: Hombre de 46 años se presentó con dolor abdominal, fiebre e ictericia. La tomografía reveló una masa en la cabeza del páncreas, asociada a calcificaciones, atrofia del páncreas distal y linfadenopatía peripancreática, lo que sugería malignidad. Durante la hospitalización para investigación diagnóstica, el paciente desarrolló colangitis. La colangiorresonancia magnética mostró una estenosis del conducto biliar común, que fue tratada mediante colangiopancreatografía retrógrada endoscópica con colocación de una prótesis biliar. La biopsia guiada por ultrasonido endoscópico fue no diagnóstica. Una laparotomía exploradora con biopsia abierta confirmó el diagnóstico de PAI relacionada con IgG4. A pesar del uso de corticosteroides, el paciente presentó un deterioro clínico progresivo, con aumento del dolor abdominal, progresión de las estenosis biliares y pérdida de peso significativa. Durante el seguimiento, los recambios de la prótesis biliar se hicieron progresivamente más difíciles debido a la acentuación de las estenosis. Una nueva biopsia guiada por ultrasonido endoscópico confirmó finalmente el diagnóstico de adenocarcinoma de páncreas. El paciente fue derivado para tratamiento con quimioterapia paliativa. Conclusión: El diagnóstico de PAI relacionada con IgG4 debe establecerse con criterios rigurosos, y la falta de respuesta al tratamiento debe motivar una reevaluación diagnóstica, como en este caso, en el que el cuadro correspondía, en realidad, a una neoplasia pancreática subyacente.
Palabras clave Pancreatitis Autoinmune; Corticoesteroides/uso terapéutico; Neoplasias Pancreáticas.
INTRODUCTION
Chronic pancreatitis (CP) is a progressive inflammatory disorder characterized by fibrotic replacement of the pancreatic parenchyma¹. Alcohol abuse remains the most prevalent etiology, though CP manifests in three principal forms: calcific, obstructive, and autoimmune pancreatitis (AIP). Autoimmune pancreatitis is further subclassified into type 1 – an immunoglobulin G4 (IgG4)-mediated, multisystem, fibroinflammatory condition affecting the pancreas, bile ducts, salivary glands, retroperitoneum, kidneys, and lymph nodes; and type 2 – or idiopathic duct-centric chronic pancreatitis, characterized by neutrophilic infiltration of pancreatic duct epithelium leading to duct obliteration and recurrent pancreatitis². Clinically, type 1 AIP most frequently presents as pancreatobiliary disease, although three other phenotypes are recognized: retroperitoneal fibrosis/aortitis, head and neck involvement, and Mikulicz syndrome³.
A diagnostically challenging case of AIP presenting with clinical and radiological features concerning for pancreatic malignancy, in which a definitive diagnosis was only achieved after the third diagnostic intervention is being reported.
The Institutional Ethics Committee of “Universidade Federal de Santa Catarina (CEP/UFSC)” approved the study, report number 7,279,269, CAAE (submission for ethical review) 82374624.0.0000.0121 in compliance with Directive 510/2016 of the Brazilian National Health Council4.
CASE REPORT
Physical examination revealed normal heart and lung sounds, and a soft, non-tender abdomen without guarding or rebound tenderness. Initial laboratory evaluation demonstrated microcytic anemia (hemoglobin 10.6 g/dL, MCV 83.1 fL) with normal leukocyte (5,430/mm³) and platelet (217,000/mm³) counts. Hepatic biochemistry revealed significant cholestasis (ALP 907 U/L, GGT 1,380 U/L) accompanied by moderate transaminitis (ALT 269 U/L, AST 70 U/L). Total and direct bilirubin levels were within the normal range (0.60 mg/dL and 0.40 mg/dL, respectively), although hypoalbuminemia (3.2 g/dL) was present. Notably, pancreatic enzymes were paradoxically normal (amylase 31 U/L, lipase 7 U/L) despite the clinical presentation. Tumor marker assessment revealed a CA 19-9 level of 41 U/mL (reference range ≤37 U/mL).
The patient brought an abdominal computed tomography (CT) scan performed one week earlier, which revealed imaging features consistent with chronic pancreatitis (CP) associated with severe exocrine pancreatic insufficiency, as evidenced by a markedly reduced fecal elastase level of 1 µg/g. The CT demonstrated diffuse pancreatic parenchymal abnormalities, including heterogeneous thickening of the pancreatic head and neck interspersed with punctate calcifications, contrasted by pronounced parenchymal atrophy in the pancreatic tail.
These alterations were accompanied by fat stranding in the surrounding adipose tissue and the presence of an elongated hypodense, hypovascular cystic lesion measuring 3.1 × 1.2 × 1.4 cm (anteroposterior × transverse × craniocaudal) located in the pancreatic head, closely abutting the main pancreatic duct. The duct itself was significantly dilated, measuring up to 0.5 cm in diameter throughout the pancreatic body. Additionally, multiple subcentimeter lymph nodes (up to 1.5 cm) were identified along the peripancreatic, periceliac, and para-aortic chains, suggestive of reactive lymphadenopathy.
During a 28-day hospitalization the patient developed jaundice, choluria, and acholic stools which, together with abdominal pain and fever, were consistent with Charcot’s triad. Magnetic resonance cholangiopancreatography (MRCP) confirmed the diagnosis of obstructive cholangitis. These findings prompted endoscopic retrograde cholangiopancreatography (ERCP), which demonstrated diffuse stricturing of the common bile duct, extending to the distal portion of the common hepatic duct, accompanied by upstream biliary dilation. A biliary stent was successfully deployed to relieve the obstruction.
Still during hospitalization, an endoscopic ultrasound-guided fine needle aspiration (EUS-FNA) of the pancreatic mass yielded no evidence of malignancy. Given the extensive and unresectable nature of the pancreatic lesion, the surgical team proceeded with an open biopsy (Figure 1). Histopathological examination revealed acute suppurative inflammation with a prominent IgG4-positive plasma cell infiltrate, rather than neoplastic tissue, while serum IgG4 levels were markedly elevated at 1,510 mg/dL (reference <135 mg/dL), confirming the diagnosis of type 1 AIP. The patient was discharged on oral prednisone 40 mg/day.
During outpatient follow-up, severe exocrine pancreatic insufficiency was confirmed, as evidenced by a fecal elastase level of 53 µg/g, and pancreatic enzyme replacement therapy was subsequently initiated. In addition, the patient underwent ERCP for biliary stent exchange every three months. Despite corticosteroid therapy, the patient exhibited progressive clinical deterioration, including worsening abdominal pain and significant weight loss. Six months after initiating corticosteroids, stent exchanges became increasingly challenging due to the progression of biliary strictures.
Subsequent CT scans demonstrated no significant changes in the pancreatic mass (Figure 2). However, magnetic resonance imaging (MRI) performed ten months after symptom onset revealed a persistent hypovascular mass with diffusion restriction in the pancreatic head and uncinate process, measuring approximately 4.9 cm in its largest diameter. This was associated with marked upstream dilation of the main pancreatic duct (up to 13 mm) and findings consistent with splenomesenteric venous junction thrombosis with collateral vessel formation, raising strong suspicion of an underlying pancreatic adenocarcinoma superimposed on focal pancreatitis.
Concordantly, serum CA 19-9 levels showed a progressive rise over six months (41 → 51 → 349 → 462 U/mL). Given these worrisome developments, another EUS-FNA was performed, and histopathological analysis confirming the diagnosis of pancreatic head adenocarcinoma (Figure 1). Following the diagnosis, the patient was referred for palliative oncological treatment with the FOLFIRINOX regimen (folinic acid, fluorouracil, irinotecan, and oxaliplatin). He remains under follow-up with both gastroenterology and oncology teams and has progressed to insulin-dependent diabetes mellitus due to pancreatic endocrine insufficiency.
DISCUSSION
Initial clinical suspicion favored pancreatic neoplasia; however, after an inconclusive EUS-guided fine needle aspiration followed by an open surgical biopsy, a definitive diagnosis of IgG4-related pancreatitis was established. The International Consensus Diagnostic Criteria (ICDC, 2010) defines AIP as a distinct form of pancreatitis characterized by: (1) obstructive jaundice with or without a pancreatic mass on imaging, (2) histopathological findings of lymphoplasmacytic infiltration and storiform fibrosis, and (3) a dramatic response to steroid therapy5. The differential diagnosis between AIP and pancreatic adenocarcinoma remains clinically challenging, as both conditions may present with identical symptoms including jaundice, weight loss, abdominal pain, and new-onset diabetes mellitus6. Epidemiological studies report a 3:1 male predominance in AIP cases7.
In this case, type 1 IgG4-mediated AIP diagnosis was supported by: (1) typical pancreatic mass features on ERCP, CT, and MRI; (2) histopathological demonstration of IgG4+ plasma cell infiltration (>10 cells/HPF); and (3) characteristic clinical presentation8. Notably, serum IgG4 levels remained within normal limits, underscoring the diagnostic complexity. First-line corticosteroid therapy was initiated, with close monitoring for therapeutic response.
The distinction between AIP and chronic pancreatitis carries significant prognostic implications, as chronic inflammatory processes may promote carcinogenesis. A systematic review and meta-analysis revealed a 9.6% prevalence of concurrent malignancy in AIP patients9. Furthermore, a prospective cohort study demonstrated that Chinese patients with IgG4-related disease (IgG4-RD) carried a 2.78-fold increased malignancy risk, particularly in the gastrointestinal tract10.
The distinction between AIP and chronic pancreatitis (CP) is crucial due to their markedly different therapeutic approaches, prognoses, and potential oncologic implications. Unlike CP, which is characterized by irreversible fibrosis, progressive exocrine and endocrine dysfunction, and commonly associated with risk factors like alcohol and smoking, AIP is an immune-mediated fibroinflammatory disorder that often responds favorably to corticosteroid therapy. Radiologically, AIP typically presents with diffuse pancreatic enlargement, a 'capsule-like' rim, and narrowing of the pancreatic duct without upstream dilatation – features that contrast with the ductal irregularities, calcifications, and focal glandular atrophy frequently seen in CP.
Serologically, elevated serum IgG4 levels and the presence of other organ involvement favor AIP, whereas CP lacks specific serologic biomarkers. Histologically, AIP is defined by dense lymphoplasmacytic infiltration, storiform fibrosis, and obliterative phlebitis – none of which are features of CP11. From a prognostic perspective, the distinction becomes even more relevant as chronic inflammation, whether autoimmune or not, has been implicated in carcinogenesis12. Interestingly, while AIP appears to be a malignancy-associated condition within the IgG4-RD spectrum, the presence of eosinophilia was inversely correlated with cancer risk, suggesting a possible protective immunologic mechanism13.
Despite standard immunosuppressive therapy, the patient exhibited progressive clinical deterioration featuring: (1) worsening biliary strictures requiring repeated stent revisions, (2) a 13 kg weight loss over six months; and (3) steadily rising CA 19-9 levels (41 → 462 U/mL). These red flags prompted an exhaustive malignancy reassessment, with the third histopathological specimen ultimately confirming pancreatic adenocarcinoma. Current management involves chemotherapy, highlighting the critical importance of persistent diagnostic reassessment in steroid-refractory cases12.
The diagnosis of IgG4-related pancreatitis requires meticulous evaluation based on a combination of key features: (1) serological markers (IgG4, total IgG, and antinuclear antibodies); (2) characteristic pancreatic parenchymal changes on cross-sectional imaging (CT or MRI) with ductal abnormalities demonstrated by endoscopic retrograde cholangiopancreatography or magnetic resonance cholangiopancreatography; (3) histopathological confirmation of pancreatic tissue infiltration; (4) involvement of other organ systems; and (5) therapeutic response to corticosteroids5.
However, as demonstrated in this case, the absence of clinical response to immunosuppressive therapy mandates immediate diagnostic reassessment, as it may indicate underlying pancreatic malignancy. It is plausible that pancreatic adenocarcinoma was already present at the initial presentation, but the diagnosis was missed because the biopsy specimens were limited to regions of autoimmune pancreatitis-related inflammation.
Emerging evidence confirms a significantly elevated risk of malignancies in patients with IgG4-related AIP, particularly within the first year following diagnosis13. In a multicenter cohort study, Shiokawa et al. demonstrated that the standardized incidence ratio (SIR) for cancer in AIP patients was 2.7 compared to the general population, with an alarming SIR of 6.1 during the first year. The relative risk of cancer at the time of AIP diagnosis was 4.9, indicating a strong temporal association. These findings suggest that a subset of AIP cases may represent a paraneoplastic phenomenon rather than a purely autoimmune disease14. Failure to recognize this association may result in the inappropriate continuation of immunosuppressive therapy, potentially allowing an underlying malignancy, such as pancreatic adenocarcinoma, to progress undiagnosed. Additionally, the observation that some cancers exhibited abundant IgG4-positive plasma cell infiltration in the tumor stroma further supports a complex interplay between tumorigenesis and immune dysregulation in IgG4-related disease14.
Recent data further emphasize that pancreatic adenocarcinoma is almost exclusively associated with type 1 AIP, the IgG4-related form. While chronic inflammation has long been recognized as a driver of carcinogenesis in chronic pancreatitis, similar mechanisms, including persistent fibroinflammatory responses and activation of oncogenic pathways such as NF-κB, are increasingly implicated in AIP-related tumorigenesis. Interestingly, malignancies in AIP are not limited to the pancreas but frequently involve extra-pancreatic sites such as the stomach, lung, and prostate. This observation reinforces the hypothesis that, in certain patients, AIP may arise as a paraneoplastic syndrome, further complicating the diagnostic landscape and underscoring the need for rigorous malignancy screening in this population15.
CONCLUSION
This case underscores the imperative for persistent histopathological reassessment in steroid-refractory cases, particularly when clinical or biochemical red flags (such as progressive weight loss, worsening biliary strictures, or rising CA19-9 levels) are present. A multidisciplinary approach combining serial imaging, advanced endoscopic techniques, and repeat tissue sampling remains crucial for accurate differentiation between inflammatory and malignant pancreatic processes.
CONTRIBUTIONS
All authors made substantial contributions to this work. Each participated in the conception or design of the study, or in the acquisition, analysis, or interpretation of data; contributed to drafting the manuscript or critically revising it with important intellectual content and approved the final version to be published.
DECLARATION OF CONFLICT OF INTERESTS
There is no conflict of interests to declare.
DATA AVAILABILITY STATEMENT
All content underlying the text of the article is contained in the manuscript.
FUNDING SOURCES
None.
REFERENCES
1. Hoffmeister A, Mayerle J, Beglinger C, et al. English language version of the S3-consensus guidelines on chronic pancreatitis: definition, aetiology, diagnostic examinations, medical, endoscopic and surgical management of chronic pancreatitis. Z Gastroenterol. 2015;53(12):1447-95. doi: https://doi.org/10.1055/s-0041-107379
2. Majumder S, Chari ST. Chronic pancreatitis. Lancet. 2016;387(10031):1957-66. doi: https://doi.org/10.1016/s0140-6736(16)00097-0
3. Nista EC, Lucia SS, Manilla V, et al. Autoimmune pancreatitis: from pathogenesis to treatment. Int J Mol Sci. 2022;23(20):12667. doi: https://doi.org/10.3390/ijms232012667
4. Conselho Nacional de Saúde (BR). Resolução n° 510, de 7 de abril de 2016. Dispõe sobre as normas aplicáveis a pesquisas em Ciências Humanas e Sociais cujos procedimentos metodológicos envolvam a utilização de dados diretamente obtidos com os participantes ou de informações identificáveis ou que possam acarretar riscos maiores do que os existentes na vida cotidiana, na forma definida nesta Resolução [Internet]. Diário Oficial da União, Brasília, DF. 2016 maio 24 [acesso 2025 abr 7]; Seção 1:44. Disponível em: http://bvsms.saude.gov.br/bvs/saudelegis/cns/2016/res0510_07_04_2016.html
5. Shimosegawa T, Chari ST, Frulloni L, et al. International consensus diagnostic criteria for autoimmune pancreatitis: guidelines of the International Association of Pancreatology. Pancreas. 2011;40(3):352-8. doi: https://doi.org/10.1097/mpa.0b013e3182142fd2
6. Baenas DF, Miretti VS, Caeiro F, Paira S. Differential diagnosis between pancreatic involvement in IgG4-related disease and pancreatic cancer. Gastroenterol Hepatol. 2021;44(2):144-55. doi: https://doi.org/10.1016/j.gastrohep.2020.05.019
7. Khandelwal A, Inoue D, Takahashi N. Autoimmune pancreatitis: an update. Abdom Radiol (NY). 2020;45(5):1359-70. doi: https://doi.org/10.1007/s00261-019-02275-x
8. Hegade VS, Sheridan MB, Huggett MT. Diagnosis and management of IgG4-related disease. Frontline Gastroenterol. 2019;10(3):275-83. doi: https://doi.org/10.1136/flgastro-2018-101001
9. Haghbin H, Chuang J, Fatim a R, et al. Correlation of autoimmune pancreatitis and malignancy: systematic review and meta-analysis. Dig Dis Sci. 2022;67(7):3252-64. doi: https://doi.org/10.1007/s10620-021-07179-9
10. Tang H, Yang H, Zhang P, et al. Malignancy and IgG4-related disease: the incidence, related factors and prognosis from a prospective cohort study in China. Sci Rep. 2020;10(1):4910. doi: https://doi.org/10.1038/s41598-020-61585-z
11. Kamisawa T, Imai M, Yui Chen P, et al. Strategy for differentiating autoimmune pancreatitis from pancreatic cancer. Pancreas. 2008;37(3):e62-7. doi: https://doi.org/10.1097/mpa.0b013e318175e3a0
12. Uchida K, Okazaki K. Current status of type 1 (IgG4-related) autoimmune pancreatitis. J Gastroenterol. 2022;57(10):695-708. doi: https://doi.org/10.1007/s00535-022-01891-7
13. Yu T, Wu Y, Liu J, et al. The risk of malignancy in patients with IgG4-related disease: a systematic review and meta-analysis. Arthritis Res Ther. 2022;24(1):14. doi: https://doi.org/10.1186/s13075-021-02652-2
14. Shiokawa M, Kodama Y, Yoshimura K, et al. Risk of cancer in patients with autoimmune pancreatitis. Am J Gastroenterol. 2013;108(4):610-7. doi: https://doi.org/10.1038/ajg.2012.465
15. Solil D, Dítě P, Kianička B, et al. Autoimmune pancreatitis as a risk factor of pancreatic cancer. Klin Onkol. 2024;37(6):420-6. doi: https://doi.org/10.48095/ccko2024420
Recebido em 10/4/2025
Aprovado em 17/6/2025
Scientific-editor: Anke Bergmann. Orcid iD: https://orcid.org/0000-0002-1972-8777
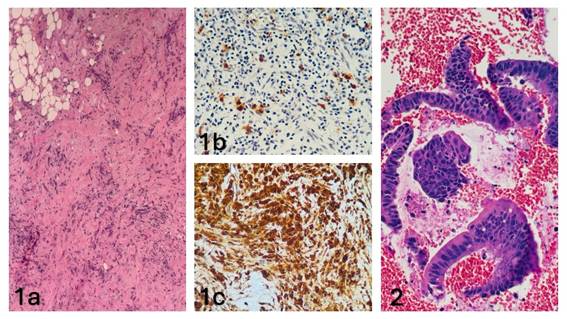
Figure 1. Histopathological and immunohistochemical features. (1a) Laparoscopic pancreatic biopsy. Fibroadipose tissue with hyalinization and dense lymphoplasmacytic infiltration (H&E, 100×). (1b) Immunohistochemical staining for IgG showing diffuse plasma cell positivity (100×). (1c) Immunohistochemical staining for IgG4 highlighting characteristic plasma cell infiltrates (200×). (2) Endoscopic ultrasound-guided fine needle aspiration (EUS-FNA) of pancreatic mass. Dissociated epithelial cell clusters demonstrating nuclear enlargement, irregular contours, hyperchromasia, and loss of polarity (H&E, 200×)
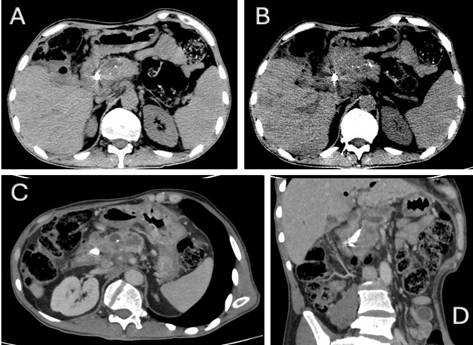
Figure 2. Contrast-enhanced abdominal computed tomography. (A) Expansile lesion with interspersed calcifications in the pancreatic head (arrow) accompanied by body atrophy. (B) Biliary stent in situ within the common hepatic duct. (C) Lesion encasing the splenomesenteric venous confluence. (D) Coronal reformat demonstrating craniocaudal tumor extent
![]()
Este é um artigo publicado em acesso aberto (Open Access) sob a licença Creative Commons Attribution, que permite uso, distribuição e reprodução em qualquer meio, sem restrições, desde que o trabalho original seja corretamente citado.